Which Sterilization Method Should I Use for My Medical Device? Complete Selection Guide
- Jan 14
- 16 min read
Choose your sterilization method based on material compatibility first, then regulatory precedent, cost, and timeline. Ethylene oxide (EO) is the most widely used method across medical devices and works for many complex, low-temperature materials, but total turnaround often takes 1–3 weeks including aeration. Steam sterilization is the fastest and least expensive, but only suitable for heat- and moisture-stable devices. Gamma radiation is effective for some polymers but can cause discoloration, embrittlement, or property changes in others. Vaporized hydrogen peroxide (VH₂O₂) is a low-temperature alternative to EO, but has limited penetration, especially for long lumens or dense packaging.
Choosing the wrong method often isn’t discovered until formal sterilization validation, at which point redesign, retesting, and revalidation can add months of delay and tens of thousands of dollars. The safest approach is to test material compatibility early and, when possible, align with the sterilization method used by your predicate device.
This guide shows you how to select the RIGHT sterilization method during early design, which materials are compatible with which methods, and how to validate your choice.

The Sterilization Decision Flowchart
Use this framework to select your method:
Question 1: Does Your Device Need to Be Sterile?
YES if:
Breaks skin barrier
Contacts normally sterile tissue or body fluids
Enters bloodstream (even indirectly)
Surgical instrument used in sterile field
Implant (any duration)
MAYBE if:
Contacts mucous membranes (may be sterile or non-sterile)
External use only but marketed with sterility claim for convenience
Used in dental procedures
NO if:
Intact skin contact only
External diagnostic device with no patient contact
Reusable device cleaned/sterilized by end-user
If NO: Skip to non-sterile pathway (cleaning validation, reusable device guidance). Rest of this guide doesn't apply.
If YES: Continue to Question 2.
Question 2: What Did Your Predicate Use?
Check predicate's 510(k) summary or labeling:
Sterilization method stated (EO, Gamma, Steam, etc.)
Sterility Assurance Level (SAL) claimed
If predicate used specific method AND your device materials similar:
Strong bias toward using same method
FDA expects equivalent or better sterilization
Validation approach proven for this device type
If predicate used different method OR you have different materials:
Can use alternative method with justification
Must demonstrate equivalence in submission
If predicate information unclear:
Research similar devices in same category
Check FDA device classification for guidance
Request Pre-Sub meeting to discuss
Question 3: Material Compatibility - First Cut
Heat-stable materials (can withstand 121-134°C steam):
Stainless steel, titanium (most metals)
Glass, ceramics
Some high-temp polymers (PEEK, PSU, PPSU)
Method: Steam sterilization (fastest, cheapest)
Heat-sensitive polymers (most medical-grade plastics):
Polyethylene (PE), polypropylene (PP)
Polycarbonate (PC), ABS
Silicones, polyurethanes
PTFE, PVC
Method: EO, Gamma, VH2O2, or E-beam
Radiation-sensitive materials:
Some polymers (PTFE yellows/embrittles, PVC degrades)
Certain lubricants and adhesives
Living tissues (allografts)
Avoid: Gamma/E-beam radiation
Complex assemblies (multiple materials + electronics):
Heat-sensitive electronics + heat-stable housing
Multiple polymers with different compatibility
Adhesives, lubricants, seals
Method: EO or VH2O2 (low temperature)
Question 4: Cost & Timeline Constraints
Need fastest validation (2-3 months):
Steam (if materials compatible)
Gamma radiation (if materials compatible)
Need lowest ongoing cost:
Steam: $0.50-$2 per unit
Gamma: $2-$8 per unit
Limited capital for validation:
Contract sterilization (any method): $15K-$40K validation
In-house steam: $50K-$100K equipment + validation
Timeline not urgent:
EO works but takes longer (7-14 day cycle)
Can afford 4-6 month validation
Question 5: Volume & Supply Chain
Low volume (<10,000 units/year):
Contract sterilization any method
Don't build in-house capability
High volume (>100,000 units/year):
Consider in-house steam (if compatible)
Contract gamma/EO for economies of scale
International distribution:
Gamma widely available globally
EO less available in some regions
Consider regulatory requirements in target markets (EU MDR restricts some EO use)
The 5 Major Sterilization Methods Explained
Ethylene Oxide (EO) - The Most Versatile
Market share: ~50% of terminally sterilized devices
How it works: EO gas penetrates packaging and materials, kills microorganisms by alkylating (chemically attacking) proteins and DNA at low temperature (37-63°C).
The process:
Pre-conditioning: 12-24 hours at controlled temperature/humidity (hydrates spores for easier kill)
Sterilization cycle: 2-4 hours EO gas exposure at 37-63°C
Aeration/degassing: 2-14 days to remove toxic EO residuals from device and packaging
Total cycle time: 3-15 days (typically 7-14 days including aeration)
Why the long aeration: EO is toxic (carcinogen). Materials absorb EO during sterilization and slowly release it. Must wait until residuals drop below ISO 10993-7 limits (typically <10 ppm EO for prolonged contact devices).
Materials compatibility:
✅ Excellent: PE, PP, PC, ABS, nylon, silicone, polyurethane, metals, glass
⚠️ Marginal: PVC (absorbs heavily - requires 21-28 day aeration), natural rubber
❌ Avoid: Certain drug coatings (may degrade)
Advantages:
Low temperature (widest material compatibility)
Excellent penetration (lumens, porous materials, complex geometries)
Works for multi-material assemblies (electronics + polymers)
Well-established (FDA very familiar)
Disadvantages:
Long cycle time (7-14 days limits manufacturing flexibility)
Toxic residuals require testing and extended aeration
Environmental/regulatory concerns (EU restrictions increasing)
Cannot sterilize liquids or biologics
Cost:
Validation: $20K-$35K
Per-unit: $3-$10 (contract sterilization)
Timeline: 4-6 months validation
Standards: ISO 11135 (EO sterilization), ISO 10993-7 (residual limits)
Best for: Heat-sensitive complex assemblies, devices with lumens, multi-material devices
Steam Sterilization (Autoclave) - Fastest & Cheapest
Market share: ~40% (dominated by reusable instruments, all-metal devices)
How it works: Saturated steam at high temperature (121-134°C) and pressure denatures proteins and disrupts microbial cell membranes. Moist heat kills 100x faster than dry heat at same temperature.
The process:
Air removal: Vacuum or gravity displacement removes air (air prevents steam contact)
Sterilization: 3-30 minutes at 121-134°C with saturated steam
Drying: 10-30 minutes (removes moisture from load)
Total cycle time: 30-90 minutes
Three cycle types:
Gravity displacement: Steam displaces air downward (simple, slower)
Pre-vacuum (Prevac): Vacuum pump removes air first (faster, better penetration, preferred for wrapped instruments)
Flash: Rapid unwrapped sterilization (immediate use)
Materials compatibility:
✅ Excellent: Stainless steel, titanium, glass, PEEK, PSU/PPSU, high-temp silicones
⚠️ Marginal: PP at 121°C (may deform under load), some high-temp nylons
❌ Incompatible: PE, standard PP, PC, ABS, PVC, acrylic, electronics, most adhesives
Critical limitation: Only 121-134°C rated materials. Most common medical polymers (PE, PP, PC, ABS) melt or deform.
Advantages:
Fastest cycle (30-90 min total)
Lowest cost ($0.50-$2 per unit)
No toxic residuals (only water vapor)
Environmentally friendly
Can be done in-house ($10K-$50K equipment)
Immediate use (no aeration)
Disadvantages:
High temperature (very limited polymer compatibility)
Moisture exposure (damages moisture-sensitive components)
Cannot sterilize electronics
Cannot sterilize most common medical plastics
Cost:
Validation: $15K-$25K (contract) or $30K-$60K (in-house)
Per-unit: $0.50-$2 (contract) or $0.10-$0.50 (in-house)
Equipment: $10K-$50K (in-house option)
Best for: All-metal devices, high-temp polymers, reusable surgical instruments, high-volume manufacturing
Gamma Radiation - High Throughput
Market share: ~25-30% (growing, especially single-use disposables)
How it works: Gamma rays from Cobalt-60 radioactive source ionize DNA causing double-strand breaks. Also creates free radicals from water that attack cellular components. Room temperature, kills through accumulated damage.
The process:
Products fully packaged, loaded onto pallets
Conveyor carries pallets past Co-60 source in shielded vault
Exposure time determines dose (typical: 25 kGy)
Products exit and release immediately (no residuals)
Total cycle time: Hours to 1-2 days (including transport)
Dose mapping required: Map radiation distribution throughout load to identify minimum dose location (Dmin - must achieve SAL) and maximum dose location (Dmax - must not damage product). Typical dose uniformity ratio: 1.2-1.5.
Materials effects:
Gamma radiation causes two competing effects in polymers:
Chain scission: Breaks polymer chains → brittleness, weakness
Cross-linking: Creates bonds between chains → stiffness
Oxidation: Free radicals + oxygen → discoloration (yellowing)
Materials compatibility:
✅ Excellent: PE (cross-links, slight yellowing acceptable), PP, nylon, silicone, metals, glass
⚠️ Marginal: PC (yellows significantly), polysulfone (discolors), ABS (discoloration), polyurethane (test specific grade)
❌ Avoid: PTFE (severe embrittlement/yellowing), PVC (degrades, releases HCl), natural rubber
Maximum dose limits:
PE, PP: 50-100 kGy (minimal effects)
PC: 25-30 kGy (yellowing acceptable to this level)
PTFE: <10 kGy (severe damage above)
Advantages:
Room temperature (no heat damage)
Excellent penetration (sterilizes through dense packaging, thick materials)
High throughput (continuous conveyor, large batches)
No residuals (immediate release)
Can process entire pallets (months of inventory at once)
Economies of scale at high volume
Disadvantages:
Discoloration (yellowing) of PC, ABS, some other polymers
Embrittlement of PTFE, PVC
Changes mechanical properties
Cannot sterilize biologics, living tissues
Radioactive source (regulatory concerns)
Limited facility locations (not in-house option)
Cost:
Validation: $20K-$30K
Per-unit: $2-$8 (much cheaper at high volume: 100K units = $2/unit)
Timeline: 3-4 months validation
Standards: ISO 11137-1, -2, -3 (radiation sterilization)
Best for: High-volume single-use devices, polymer-based products (if material compatible), when fast post-packaging turnaround needed
Vaporized Hydrogen Peroxide (VH2O2) - EO Alternative
Market share: ~5% (growing as EO replacement)
How it works: H2O2 vapor oxidizes microbial components through free radical formation (•OH, •HO2). Decomposes naturally to water and oxygen (no toxic residuals). Works at low temperature (40-60°C).
The process:
Conditioning: Remove moisture (10-30 min) - H2O2 competes with water
Vaporization: Liquid H2O2 vaporized into chamber (30-60 min)
Sterilization: 30-90 min exposure at 40-60°C
Aeration: 10-30 min (H2O2 decomposes naturally)
Total cycle time: 2-4 hours
Critical limitation - penetration:
H2O2 vapor cannot penetrate:
Small lumens (<1-2mm diameter)
Long narrow channels
Tightly packed loads
Also cannot penetrate/compatible with:
❌ Cellulosics (paper, cardboard, cotton) - absorb H2O2
❌ Natural rubber - absorbs H2O2
❌ Long/narrow lumens - vapor cannot reach
Materials compatibility:
✅ Excellent: PE, PP, PC, ABS, acrylics, silicones, metals, glass, electronics
⚠️ Marginal: Some nylons (can absorb)
❌ Incompatible: Cellulosics, paper packaging, natural fibers, long small-diameter lumens
Advantages:
Low temperature (40-60°C, electronics compatible)
Fast cycle (2-4 hours vs. EO's 7-14 days)
No toxic residuals (decomposes to H2O + O2)
Environmentally friendly
No extended aeration needed
EU regulatory preference over EO
Disadvantages:
Limited penetration (cannot penetrate lumens <1mm)
Incompatible with cellulosics (limits packaging options)
Cannot sterilize liquids
Smaller chamber size than EO
More expensive per unit than EO
Newer method (less historical data)
Cost:
Validation: $25K-$40K
Per-unit: $5-$15
Equipment: $100K-$300K (in-house possible but expensive)
Standards: ISO 14937 (general sterilizing agents - no VH2O2-specific standard yet)
Best for: EO alternative where penetration not critical, electronics, EU market, when faster turnaround than EO needed
Electron Beam (E-Beam) - Fast Radiation Alternative
Market share: ~3-5%
How it works: Same as gamma (ionizing radiation damages DNA, creates free radicals) but uses accelerated electrons instead of Co-60. Can turn beam on/off. Room temperature.
Critical difference from gamma: Limited penetration
Electrons have mass (gamma photons don't)
Maximum penetration: 4-6 cm depending on energy and material density
Thick products require two-sided exposure
The process:
Products on conveyor pass under electron beam
Beam scanned across conveyor width
Exposure time (conveyor speed) determines dose
Thick products: flip and second pass, or dual beams (top/bottom)
Total cycle time: Minutes to hours
Materials compatibility: Identical to gamma
Same chain scission, cross-linking, oxidation effects
Same material restrictions (PTFE, PVC problematic; PE, PP good)
Advantages:
Very fast processing (seconds exposure time)
Room temperature
No radioactive source (better public perception)
Can turn on/off (safety, control)
Precise dose control
Immediate release
Disadvantages:
Limited penetration (4-6 cm max)
Requires two-sided exposure for thick products
Material effects same as gamma (yellowing, embrittlement possible)
High capital cost ($3-10M equipment)
Limited facility locations
Cost:
Validation: $20K-$35K
Per-unit: $3-$10 (similar to gamma)
Timeline: 3-4 months validation
Standards: ISO 11137 (same as gamma)
Best for: Thin/flat devices (syringes, tubing, films), when gamma facility not accessible, preference for non-radioactive method
Material Compatibility: The Critical Tables
Use these tables to make initial method selection based on materials:
Common Medical Polymers
Material | Steam 121°C | Steam 134°C | EO | Gamma | VH2O2 | Notes |
Polyethylene (PE) | ❌ No | ❌ No | ✅ Yes | ✅ Yes | ✅ Yes | Most common choice: EO or Gamma |
Polypropylene (PP) | ⚠️ Marginal | ❌ No | ✅ Yes | ✅ Yes | ✅ Yes | Can withstand 121°C if stabilized |
Polycarbonate (PC) | ❌ No | ❌ No | ✅ Yes | ⚠️ Yellows | ✅ Yes | Gamma causes yellowing |
ABS | ❌ No | ❌ No | ✅ Yes | ⚠️ Discolors | ✅ Yes | Gamma may discolor |
Nylon (PA) | ⚠️ Some grades | ❌ No | ✅ Yes | ✅ Yes | ⚠️ Absorbs | High-temp nylons ok for steam |
PEEK | ✅ Yes | ✅ Yes | ✅ Yes | ✅ Yes | ✅ Yes | Excellent all-around |
PSU/PPSU | ✅ Yes | ✅ Yes | ✅ Yes | ⚠️ Discolors | ✅ Yes | Great for reusable instruments |
PVC | ❌ No | ❌ No | ⚠️ Long aeration | ⚠️ Degrades | ✅ Yes | Avoid EO if possible |
PTFE (Teflon) | ✅ Yes | ✅ Yes | ✅ Yes | ❌ Severe damage | ✅ Yes | Never use gamma |
Silicone | ⚠️ Grade dependent | ⚠️ Grade dependent | ✅ Yes | ✅ Yes | ✅ Yes | Verify temp rating for steam |
Polyurethane | ❌ No | ❌ No | ✅ Yes | ⚠️ Variable | ✅ Yes | Test gamma on specific grade |
Legend:
✅ Yes - Generally compatible
⚠️ Marginal - Test specific grade/formulation
❌ No - Avoid this method
Metals
Material | Steam | EO | Gamma | VH2O2 |
Stainless Steel | ✅ Ideal | ✅ Yes | ✅ Yes | ✅ Yes |
Titanium | ✅ Ideal | ✅ Yes | ✅ Yes | ✅ Yes |
Aluminum | ✅ Yes | ✅ Yes | ✅ Yes | ✅ Yes |
Brass/Copper | ⚠️ May tarnish | ✅ Yes | ✅ Yes | ✅ Yes |
Chrome plating | ✅ Yes | ✅ Yes | ✅ Yes | ✅ Yes |
Note: Metals generally compatible with all methods. Steam preferred for all-metal devices (cost, speed).
Other Materials
Material | Steam | EO | Gamma | VH2O2 |
Glass | ✅ Yes | ✅ Yes | ✅ Yes | ✅ Yes |
Ceramics | ✅ Yes | ✅ Yes | ✅ Yes | ✅ Yes |
Paper/cardboard | ❌ No | ✅ Yes | ✅ Yes | ❌ Absorbs H2O2 |
Natural rubber | ❌ No | ⚠️ Degrades | ⚠️ Degrades | ❌ Absorbs |
Adhesives | ⚠️ Many fail | ⚠️ Test specific | ⚠️ Test specific | ⚠️ Test specific |
Lubricants | ⚠️ May migrate | ⚠️ May migrate | ⚠️ May degrade | ✅ Generally ok |
Electronics | ❌ No | ⚠️ If <63°C | ⚠️ Some damage | ✅ Best choice |
Cost & Timeline Comparison
Validation Costs (First Time):
Method | Validation Cost | Timeline | Notes |
Steam | $15K-$25K (contract) $30K-$60K (in-house) | 2-3 months | Fastest validation |
EO | $20K-$35K | 4-6 months | Includes EO residual testing |
Gamma | $20K-$30K | 3-4 months | Includes dose mapping |
VH2O2 | $25K-$40K | 3-5 months | Newer method, more validation work |
E-Beam | $20K-$35K | 3-4 months | Similar to gamma |
Per-Unit Costs (Contract Sterilization):
Method | Cost per Unit | Volume Sensitivity |
Steam | $0.50-$2 | Low (fairly flat pricing) |
EO | $3-$10 | Moderate (decreases with volume) |
Gamma | $2-$8 | High (much cheaper at high volume) |
VH2O2 | $5-$15 | Moderate |
E-Beam | $3-$10 | High (economies of scale) |
Cycle Times (Production):
Method | Cycle Time | Throughput Impact |
Steam | 1 hour | Can run multiple cycles/day |
EO | 7-14 days | Limits production flexibility |
Gamma | 1-2 days | Can process large batches |
VH2O2 | 2-4 hours | Moderate flexibility |
E-Beam | Minutes-hours | High throughput |
Sterilization Validation Requirements by Method
All terminal sterilization methods require validated processes under 21 CFR 820.75 (process validation) and are commonly executed using FDA-recognized consensus standards (ISO/ANSI/AAMI), depending on the modality.
Three Validation Phases (Common Industry Structure Across Methods)
Installation Qualification (IQ): Document sterilizer equipment and installation, verify calibration status, and confirm setup matches manufacturer specifications.
Operational Qualification (OQ): Demonstrate the process runs within defined operating limits (for example temperature, pressure, gas concentration), identify worst-case locations, and lock cycle parameters.
Performance Qualification (PQ): Demonstrate the validated process consistently achieves the target sterility outcome across multiple successful runs, often 3 consecutive cycles, using biological indicators and product assessments to confirm no unacceptable damage or degradation.
Sterility Assurance Level (SAL)
For many terminally sterilized medical devices, the commonly targeted SAL is 10⁻⁶, but the validation approach should match the sterilization modality and device risk profile.
EO-Specific Validation (Ethylene Oxide)
Additional requirements typically include:
EO residual evaluation per ISO 10993-7, measuring EO and key byproducts (including ECH and EG), and demonstrating residuals are below allowable limits based on device contact category and patient exposure. Avoid using generic ppm numbers unless tied to a specific table and device category.
Process characterization including conditioning controls (temperature, humidity), gas concentration management, and aeration effectiveness.
Gamma / E-beam Validation
Additional requirements typically include:
Dose mapping and dose-setting per ISO 11137, establishing minimum dose for sterility and maximum dose your product can tolerate without performance degradation.
25 kGy is a common industry reference point, but the validated dose must be justified by your product-specific dose-setting approach (bioburden, load configuration, dose distribution).
Steam Validation
Cycle selection (gravity, pre-vacuum, steam-flush pressure-pulse) based on packaging and load configuration.
Process monitoring using appropriate indicators, with Geobacillus stearothermophilus commonly used for steam biological indicators.
VH2O2 Validation (Vaporized Hydrogen Peroxide)
Establish and validate process parameters (concentration, time, temperature, humidity, vacuum as applicable).
Key challenge is demonstrating effective exposure to all device surfaces, especially long or narrow lumens and complex internal channels, where penetration limits can drive method choice.
Testing Compatibility Before You Commit
A small feasibility exposure study early can prevent expensive redesign and revalidation later. Do not wait until formal sterilization validation to learn that your materials, adhesives, seals, or electronics degrade under your chosen method.
Phase 1: Material Screening (Early Development)
When: During material selection, well before design freeze
What to do: Run worst-case sterilization exposure cycles (or feasibility studies) for each short-listed method using representative material coupons or simple components.
What to measure:
Dimensional stability (warping, shrinkage)
Appearance changes (yellowing, discoloration)
Mechanical property shifts (tensile strength, impact resistance)
Surface changes (cracking, crazing)
Tip: If you are deciding between multiple methods, this is where you eliminate the “obviously incompatible” ones quickly, before your design locks in.
Phase 2: Component and Subassembly Checks (Mid Development)
When: After key components are defined, before full device build
What to do: Sterilize representative subassemblies and confirm critical interfaces survive exposure.
Check:
Adhesive bonds and seal integrity
Moving parts friction and function
Dimensional fit across mating parts
Material interactions (stress cracking, leaching risks)
Phase 3: Production-Equivalent Verification (Pre Validation)
When: After design freeze, before formal validation
What to do: Sterilize multiple production-equivalent units, then re-run the same functional and performance checks you plan to claim in your submission. Justify sample size based on risk and verification strategy.
This is your practical go or no-go checkpoint before you spend on full validation cycles and documentation.
Common Sterilization Failures & How to Avoid Them
Sterilization failures are a major source of validation delays and rework. These failures usually stem from incompatibilities between sterilization method, materials, geometry, or packaging — not because the sterilization process itself is deficient. Here are the most common failure modes and how to prevent them.
Failure #1 — Material Incompatibility Discovered Late
Scenario:
A PC (polycarbonate) device housing successfully met functional specs, but final gamma sterilization caused yellowing and increased brittleness.
Root cause:
Some polymers, including PC and ABS, can undergo radiation-induced discoloration or embrittlement under gamma or e-beam exposure.
Fix:
Select a sterilization method compatible with your materials, then verify with early feasibility or exposure testing.
Prevention:
Conduct sterilization exposure cycles on material coupons early (Phase 1 material screening).
Use feasibility screening to eliminate incompatible methods before design is locked.
Failure #2 — EO Residuals Exceed Acceptable Levels
Scenario:
PVC components passed sterilization, but residuals remained high after prolonged aeration, delaying manufacturing release.
Root cause:
Certain materials absorb ethylene oxide and release it slowly, resulting in residual levels above allowable thresholds for the device’s intended contact category.
Fix:
Either adjust aeration protocols or substitute incompatible materials.
Prevention:
Evaluate EO residuals per ISO 10993-7 with material-specific exposure data.
Avoid polymers with high adsorption/absorption if EO is planned.
Failure #3 — Steam Sterilization Warping Components
Scenario:
A tight-tolerance PP housing shrank during steam sterilization, preventing correct assembly.
Root cause:
Heat and moisture from steam can cause some polymers to shrink, warp, or relax stress, especially at high temperatures.
Fix:
Rework design tolerances or choose more steam-stable materials.
Prevention:
Early material exposure testing at sterilization temperatures.
Account for thermal expansion and moisture effects in design controls.
Consider dimensionally stable polymers (e.g., PEEK, PSU) if steam is required.
Failure #4 — VH₂O₂ Cannot Penetrate Internal Voids
Scenario:
A device with a small internal lumen (<1–2 mm diameter) showed incomplete sterilization after VH₂O₂ exposure.
Root cause:
Vaporized hydrogen peroxide (VH₂O₂) has limited penetration into small, long internal channels or lumens.
Fix:
Switch to a sterilization method with better penetration (e.g., EO) or redesign geometry.
Prevention:
Evaluate sterilant penetration in Phase 1/2 exposure screening.
Understand geometry limits for your selected sterilant and correlate with worst-case device paths.
Failure #5 — Adhesive Bond Failure After Sterilization
Scenario:
A UV-cure adhesive used to join two components lost most of its bond strength after EO exposure, causing in-service failure.
Root cause:
Many adhesives and encapsulants are sensitive to sterilization conditions (heat, chemistry, radiation), weakening or softening.
Fix:
Replace with a sterilization-compatible adhesive or redesign with mechanical locking features.
Prevention:
Include adhesives in material screening and subassembly exposure tests.
Confirm adhesive integrity after your planned sterilization exposure.
Failure #6 — Packaging Seal Failure
Scenario:
A Tyvek pouch used to package devices for steam sterilization showed a high incidence of seal failures.
Root cause:
Packaging that hasn’t been validated for your selected sterilization cycle can fail due to temperature, pressure, or moisture.
Fix:
Re-qualify seals using your sterilization method, or choose packaging designed for that cycle.
Prevention:
Treat packaging validation as an integral part of overall sterilization validation (ISO 11607 alignment).
Include seal integrity, barrier performance, and aging in pre-validation checklists.
Critical Takeaways
Test material compatibility in Month 3-4, not Month 17. $2K early testing prevents $80K redesign + 6-month delay.
Use predicate's method if materials similar. FDA expects equivalent or better. Proven approach for your device type.
Steam is best IF materials compatible. Fastest (1 hr), cheapest ($0.50-$2/unit), shortest validation (2-3 months). Only works for heat-stable materials.
EO is most versatile but slowest. Works for 50% of devices, excellent penetration, but 7-14 day cycle limits manufacturing flexibility.
Gamma causes discoloration. Test on YOUR specific material. PC yellows, PTFE severe damage. PE, PP generally ok.
VH2O2 cannot penetrate small lumens (<1mm). Use EO if penetration critical.
PVC + EO = 21-28 day aeration. Avoid PVC if using EO.
Always test full device performance AFTER sterilization. Passing sterilization ≠ device still works.
Package validation is part of sterilization validation. Seals must survive sterilization exposure.
Contract sterilization for most devices. Only consider in-house for steam + high volume (>50K units/year).
The Fastest Path to Market
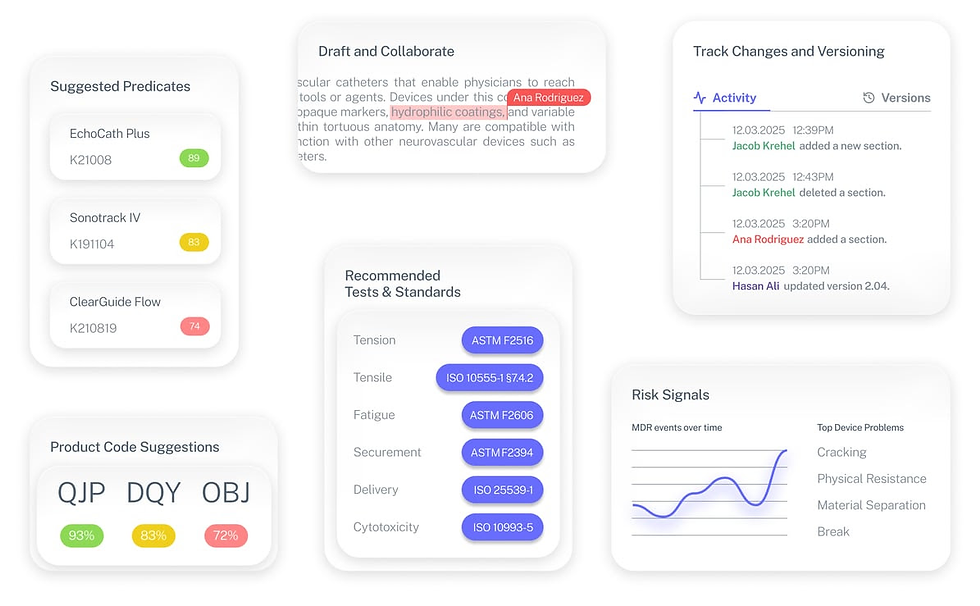
No more guesswork. Move from research to a defendable FDA strategy, faster. Backed by FDA sources. Teams report 12 hours saved weekly.
FDA Product Code Finder, find your code in minutes.
510(k) Predicate Intelligence, see likely predicates with 510(k) links.
Risk and Recalls, scan MAUDE and recall patterns.
FDA Tests and Standards, map required tests from your code.
Regulatory Strategy Workspace, pull it into a defendable plan.
👉 Start free at complizen.ai
Frequently Asked Questions
Can I change sterilization methods after FDA clearance?
Often, yes, but you may need a new 510(k) if the change could significantly affect safety or effectiveness, for example, changing from EO to radiation can impact materials, packaging, or residual risk. If your risk-based assessment shows no significant impact, you may document the change in your design controls instead.
What if my predicate used a sterilization method I can’t use?
You can use a different method if you validate sterility and show the method does not introduce new risks, including device and packaging compatibility impacts. In your 510(k), clearly explain the method, validation approach, SAL, and any compatibility testing that supports equivalence.
How do I know if my material is compatible with a sterilization method?
Start with supplier data and predicate precedent, then confirm with your exact material grade, additives, and final manufacturing process. A quick screening exposure with a contract sterilizer is a strong way to de-risk method selection before full validation.
Can I sterilize my device multiple times?
Only if it’s intended and labeled as reusable. Reusable devices must validate that the reprocessing instructions work as labeled, and that device performance remains acceptable over the maximum number of cycles claimed in labeling.
What’s the difference between sterilization and disinfection?
Sterilization is intended to eliminate all forms of microbial life, including highly resistant organisms like bacterial spores. Disinfection reduces microbial contamination, but many disinfection processes are not reliably sporicidal, which is why devices contacting sterile tissue or the bloodstream typically require sterilization.
How long does sterilization validation take?
It varies by device complexity, supplier backlog, and method. In general, EO can take longer because aeration and residual considerations may be needed, while steam and radiation methods can be faster once compatibility is proven and the process is defined.
Can I use the same validation for different product sizes?
Sometimes. A worst-case “product family” approach can work when products share the same materials, packaging configuration, and sterilization challenge characteristics, and you can justify worst-case selection.
What if my device fails sterilization validation?
Corrective actions depend on why it failed. Lethality failures may require cycle parameter changes and requalification. Residual issues may require aeration or material changes. Device damage often forces a material or method change, followed by revalidation.
Do I need to revalidate sterilization periodically?
You must maintain routine control and typically perform periodic review or requalification per your quality system and the sterilization standard. You also reassess validation when changes occur, for example, materials, packaging, load configuration, site, or process parameters.
Can I sterilize in-house vs. using a contract sterilizer?
Most companies use contract sterilizers. In-house sterilization is most feasible for steam when volumes and facilities justify it. EO and radiation methods typically require specialized infrastructure and controls, so they are commonly outsourced.
What documentation do I need for my 510(k) submission?
Include sterility information consistent with FDA’s sterility submissions guidance, covering the method, standards used, SAL, validation approach, and any method-specific elements such as EO residual considerations where applicable.
How does sterilization affect shelf life?
Shelf life is supported by package integrity plus device and material stability over time. Accelerated aging can support shelf-life claims, but you still need to show the sterile barrier and device performance remain acceptable through end-of-shelf-life.
Can I sterilize drugs or biologics with my device?
Drug or biologic components may be sensitive to heat or radiation, which can drive method selection and sometimes requires additional FDA interaction. For combination products, engage FDA early when sterilization could affect the drug or biologic component.



