What Is FDA's Breakthrough Devices Program? Complete 2025 Guide
- Jun 25, 2025
- 6 min read
Updated: Sep 7, 2025
The FDA Breakthrough Devices Program gives truly novel, life-saving technologies a faster lane through 510(k), De Novo or PMA review. As of 30 September 2024 the agency had granted 1,041 designations, but only 128 devices have reached the U.S. market so far.
Designated sponsors gain:
Priority FDA access – direct, rapid dialogue with senior reviewers and shorter review queues.
Meaningful—but variable—speed – a recent FOIA study shows a ~75-day average review-time saving, not the six-to-twelve months sometimes advertised.
Potentially quicker Medicare coverage via CMS’s new TCET process (still voluntary and evidence-dependent).
This comprehensive guide reveals qualification criteria, application strategies, and realistic expectations for the Breakthrough Devices Program—helping you determine if your device qualifies and how to maximize your competitive advantage.

What Is FDA's Breakthrough Devices Program?
The Breakthrough Devices Program is FDA's expedited pathway for medical devices that provide more effective treatment or diagnosis of life-threatening or irreversibly debilitating conditions.
Launched in 2018, the program replaced the Expedited Access Pathway and gives qualifying devices priority status throughout the entire FDA review process. It's available for 510(k) clearance, De Novo classification, PMA approval, and device-led combination products.
Core Program Benefits
Interactive Communication: Direct access to FDA experts throughout device development, including expedited pre-submission meetings and Q-submission responses.
Priority Review: Marketing submissions (510(k), De Novo, PMA) jump to the head of the queue, potentially reducing timelines by 6-12 months.
Flexible Study Design: FDA provides guidance on efficient clinical trial approaches and may accept novel endpoints or study designs.
Post-Market Emphasis: Greater reliance on post-market data collection versus extensive pre-market requirements when scientifically appropriate.

Do You Qualify? Breakthrough Designation Criteria
Primary Requirement (Must Meet)
Your device must provide more effective treatment or diagnosis of a life-threatening or irreversibly debilitating disease or condition.
"More effective" means clinically meaningful improvement over existing alternatives, addressing previously unmet medical needs, or providing significant advantages in treatment outcomes.
Secondary Criteria (Must Meet At Least One)
1. Represents Breakthrough Technology
Novel device type, mechanism of action, or approach that offers significant improvement over existing approved alternatives. Not necessarily "first-of-its-kind" but meaningfully different.
2. No Approved Alternatives Exist
No existing FDA-approved/cleared devices for the specific indication, existing devices are inadequate for the patient population, or current standard of care is non-device based.
3. Offers Significant Advantages
Demonstrates more effective treatment or diagnosis compared to existing approved/cleared alternatives with clinically meaningful benefits to patients.
4. Device Availability Benefits Patients
Addresses critical unmet medical need where benefits outweigh risks for target population, representing important public health consideration.
2023 Expanded Eligibility
Updated guidance includes devices addressing healthcare disparities, non-addictive products for pain management, and devices for addiction treatment.

What Are Your Real Chances? Program Statistics
Designation Success Rates
As of September 2024:
1,041 devices received breakthrough designation
128 devices achieved clearance/approval
~12% approval rate from designation to market
913 devices still in development or discontinued
Timeline Reality
FDA processes designation requests within 60 days.
If additional information is needed, FDA typically requests it within 30 days of receiving your submission.
Review acceleration varies by pathway:
PMA submissions: 6-12 months faster
De Novo requests: 8-15 months typical vs. standard timeline
510(k) submissions: Minimal acceleration (already fast)
Why Devices Don't Reach Market
Analysis shows designated devices fail to reach market due to development challenges, funding issues, or clinical trial setbacks—not regulatory barriers. Breakthrough designation makes FDA approval easier, not product development easier.
What Makes Devices Win Breakthrough Status?
Strong Applications Share Common Elements
Clear Unmet Need Documentation: Specific patient populations, quantified disease burden, and gaps in current treatment options with supporting clinical literature.
Compelling Preliminary Evidence: Early clinical data, robust preclinical studies, or published research demonstrating device potential and technical feasibility.
Well-Defined Regulatory Strategy: Clear pathway identification (510(k), De Novo, PMA) with understanding of evidence requirements and development timeline.
Active FDA Engagement Plan: Commitment to participate in meetings, respond to guidance, and maintain communication throughout development process.
Is Breakthrough Designation Worth It? Strategic Analysis
Immediate Competitive Advantages
Faster Market Access: 6-12 month acceleration translates to earlier revenue recognition and competitive positioning advantages.
Regulatory Efficiency: FDA guidance prevents costly late-stage protocol changes and reduces regulatory uncertainty.
Investment Appeal: Breakthrough status provides third-party validation of innovation and market potential for investors.
Reimbursement Fast Track: CMS's Transitional Coverage for Emerging Technologies (TCET) can provide Medicare coverage within 6 months versus typical 5-year process.
Hidden Costs and Considerations
Increased Scrutiny: Some regulatory consultants report FDA places additional requirements on breakthrough devices due to enhanced oversight and public visibility.
Resource Commitment: Enhanced FDA engagement requires dedicated regulatory resources and executive attention throughout development.
Public Expectations: Breakthrough status creates higher performance expectations from patients, providers, and media.
How to Apply: Best Practice Tips
Pre-Application Preparation (4-6 Weeks)
Market Analysis Document existing treatment options and their specific limitations with clinical data. Quantify unmet medical need using epidemiological data and patient outcome studies.
Evidence Compilation Gather preliminary clinical data, strong preclinical evidence, and published literature supporting your device approach and clinical benefits.
Competitive Assessment Analyze similar devices and their regulatory status. Identify gaps in current solutions that your device addresses.
Application Components
Device Description (2-3 pages) Detailed technical specifications, mechanism of action, intended use statement, and target patient population with clear classification rationale.
Clinical Need Justification (3-4 pages) Epidemiology of target condition, current treatment limitations with specific outcome data, healthcare disparities or access issues if applicable.
Breakthrough Criteria Analysis (4-5 pages) Point-by-point analysis demonstrating how device meets primary criterion and at least one secondary criterion with supporting clinical evidence.
Development Plan (2-3 pages) Planned clinical studies with timeline, regulatory pathway strategy, risk management approach, and post-market surveillance plan.
Optimal Submission Timing
Best Window: During device development phase after proof-of-concept but before pivotal studies, when preliminary evidence exists but FDA guidance can still influence study design.
Critical Deadline: Must submit before marketing application. FDA won't review requests received with or after PMA, 510(k), or De Novo submissions.
Common Application Mistakes That Cause Rejections
Weak Unmet Need Arguments
Problem: Generic statements about "improving patient outcomes" without specific clinical evidence or quantified patient populations.
Solution: Provide specific outcome measures, patient numbers affected, and clinical literature documenting treatment gaps.
Technology Focus vs. Clinical Benefit
Problem: Emphasizing technical innovation rather than demonstrating clinical advantages and patient benefits.
Solution: Lead with clinical outcomes and patient impact, using technology features to support clinical benefit claims.
Inadequate Competitive Analysis
Problem: Failing to demonstrate clear advantages over existing FDA-approved alternatives with specific comparative data.
Solution: Direct comparison tables showing clinically meaningful differences in outcomes, safety, or usability.
Poor Evidence Quality
Problem: Relying on theoretical benefits without supporting preliminary data or robust preclinical evidence.
Solution: Provide compelling early clinical data, comprehensive preclinical studies, or strong published literature support.
Timing Errors
Problem: Applying too early (no supporting data) or too late (development complete, no benefit from FDA guidance). Solution: Apply when preliminary evidence exists but FDA input can still influence development strategy.
Your Next Steps: Claiming Your Regulatory Advantage
The Breakthrough Devices Program represents one of medtech's most underutilized competitive advantages. While most companies focus on product development, breakthrough designation offers regulatory acceleration that can provide transformational business impact.
Most companies that qualify never apply because they underestimate their chances or overestimate the complexity. The qualification criteria aren't as restrictive as many assume, and the application process, while requiring careful preparation, offers exceptional return on investment.
Action Plan:
Complete qualification assessment using our decision framework
Compile supporting evidence for your breakthrough case
Engage regulatory expertise for application strategy and preparation
Submit before marketing application to maximize timeline benefits
The Fastest Path to Market
No more guesswork. Move from research to a defendable FDA strategy, faster. Backed by FDA sources. Teams report 12 hours saved weekly.
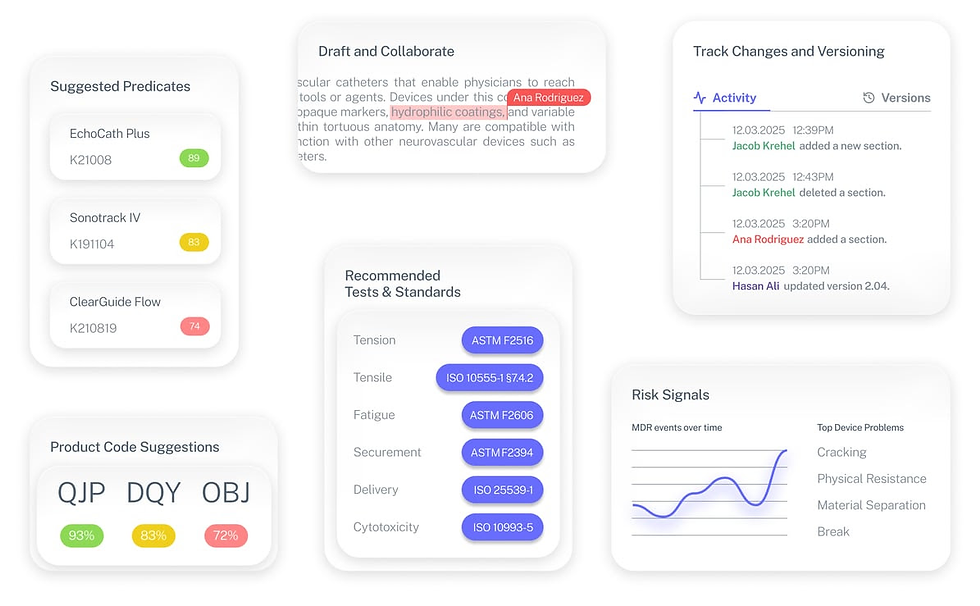
FDA Product Code Finder, find your code in minutes.
510(k) Predicate Intelligence, see likely predicates with 510(k) links.
Risk and Recalls, scan MAUDE and recall patterns.
FDA Tests and Standards, map required tests from your code.
Regulatory Strategy Workspace, pull it into a defendable plan.
👉 Start free at complizen.ai
Frequently Asked Questions
Q:What happens if my breakthrough application gets denied?
A: Denial doesn't affect your ability to submit through standard regulatory pathways. FDA provides reasoning for denial, which can help improve your overall regulatory strategy. You cannot resubmit unless there are significant device changes or new clinical evidence.
Q: How much does breakthrough designation actually speed up review?
A: Acceleration varies significantly by pathway. PMA and De Novo reviews typically see 6-12 month acceleration, while 510(k) benefits may be minimal since standard review times are already relatively short. The greater benefit often comes from FDA guidance preventing delays.
Q: Do I need completed clinical studies to apply?
A: No. You need compelling evidence of clinical benefit, which could be preliminary clinical data, robust preclinical studies, or strong published literature supporting your approach. The key is demonstrating reasonable expectation of clinical success.
Q: Can breakthrough devices use expedited Medicare coverage?
A: Yes. CMS's Transitional Coverage for Emerging Technologies (TCET) program specifically leverages FDA breakthrough designation for expedited coverage decisions, potentially providing reimbursement within 6 months versus the typical 5-year process.
Q: What if my device doesn't seem "breakthrough" enough?
A: Many qualifying devices aren't revolutionary technology but rather better solutions to existing problems. Focus on clinical benefits and patient outcomes rather than technical novelty. If your device more effectively addresses an unmet medical need, you likely qualify.


