How to Build a Medical Device Regulatory Strategy: Complete Guide
- Beng Ee Lim

- Nov 10, 2025
- 16 min read
A medical device regulatory strategy is your comprehensive plan for achieving FDA clearance or approval. It includes device classification, pathway selection (510(k), De Novo, or PMA), resource planning (team, budget, consultants), timeline mapping, testing strategy, and risk mitigation. Build it during concept phase—before design freeze or testing begins—to avoid expensive mistakes and accelerate market entry.
Companies that build regulatory strategy during concept phase make smarter pathway decisions, secure funding faster, and avoid the $500K+ mistakes that derail 40% of first-time submissions. This guide provides the frameworks for conducting regulatory feasibility assessments, evaluating pathway options, planning resources strategically, and building defensible regulatory roadmaps that accelerate market entry.

Why You Need Regulatory Strategy Before Development
Most medical device companies make the same expensive mistake: they develop their product, then figure out regulatory requirements. This backwards approach leads to design changes, redundant testing, missed deadlines, and funding shortfalls.
The cost of late regulatory planning:
Design changes mid-development: Retrofitting design controls costs 3-5x more than building them from day one
Redundant testing: Companies waste $50K-$200K on tests that don't align with FDA requirements
Pathway mistakes: Choosing wrong pathway (or wrong predicate) adds 6-12 months and forces resubmission
Funding gaps: Running out of money during FDA review because total costs were underestimated by 2-3x
Regulatory strategy determines:
Development timeline: PMA requires 3-5 years; 510(k) requires 12-24 months
Total budget: Class III PMA costs $5M-$119M; Class II 510(k) costs $500K-$2M
Funding strategy: Regulatory milestones define Series A and Series B timing
Market entry sequencing: US-first versus EU-first affects competitive positioning
Team requirements: Some pathways require full-time regulatory staff; others don't
The companies that succeed fastest conduct regulatory feasibility assessments during concept phase, integrate regulatory requirements into development planning, and build defensible strategies before committing to expensive testing.
💡 Complizen Advantage:
Before you spend a dollar on testing, Complizen helps you identify your product code, map potential predicates, estimate FDA timelines, and calculate total test and submission costs based on real predicate data.
It’s like having a regulatory feasibility assessment on day one — so your R&D, investors, and roadmap are aligned from the start.
Stage 1: Regulatory Feasibility Assessment
Before you commit to a device concept, conduct a regulatory feasibility assessment to identify red flags that could make your device economically unviable or impossible to clear.
How Do I Assess Regulatory Feasibility?
Regulatory feasibility answers one critical question: Can we get this device through FDA at a cost and timeline that makes business sense?
Step 1: Preliminary Classification
Determine likely device classification based on intended use and risk level. Your classification drives everything else in your regulatory strategy.
Search FDA's Product Classification Database for devices with similar intended use. Look for:
Product code (21 CFR regulation number)
Device class (I, II, or III)
Regulatory pathway (510(k), De Novo, PMA, or exempt)
Special controls or guidance documents
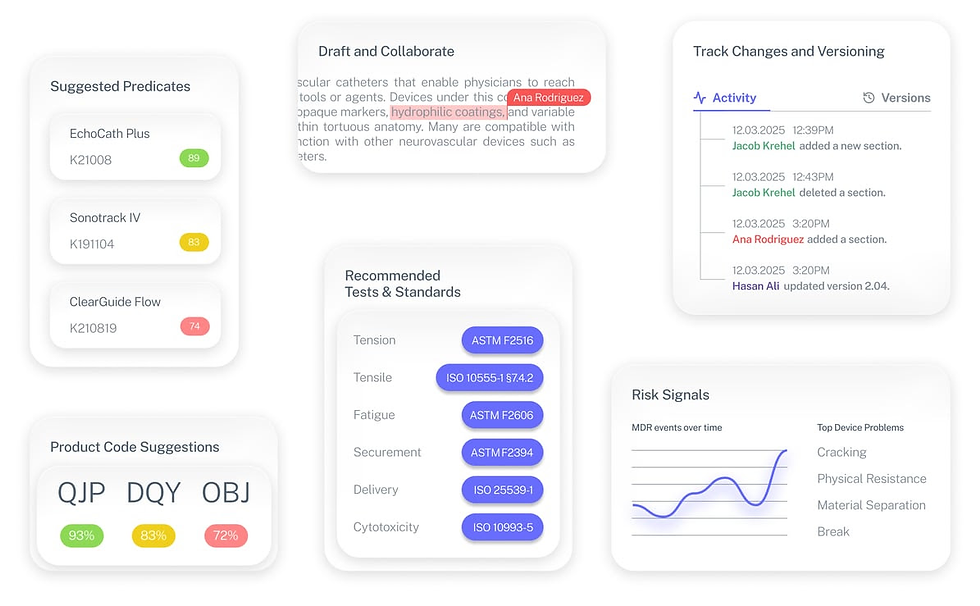
Many companies waste weeks manually searching FDA databases to find their classification. Complizen's Product Code Finder automates this discovery, identifying relevant product codes and historical 510(k) precedents in minutes instead of days.
Step 2: Predicate Analysis (for 510(k) pathway)
If pursuing 510(k), identify potential predicate devices with:
Same intended use as your device
Similar technological characteristics (or different characteristics that don't raise new safety questions)
Currently marketed (not recalled or withdrawn)
Strong 510(k) summary with clear substantial equivalence arguments
Search the FDA 510(k) database for cleared devices matching your product code. Review their 510(k) summaries to understand FDA's expectations for substantial equivalence arguments.
Instead of manually searching across multiple FDA databases, Complizen's Predicate Intelligence surfaces relevant 510(k)s with their summaries, testing data, and recognized standards—turning weeks of research into strategic decisions in hours.
Step 3: Clinical Data Requirements
Assess whether your pathway requires clinical trials:
510(k) pathway: Usually bench testing + literature review sufficient (no clinical trials)
De Novo pathway: Sometimes requires limited clinical data depending on special controls
PMA pathway: Always requires extensive clinical trials (often 100+ patients)
Clinical trials are the largest cost driver in medical device development. If your device requires PMA with clinical trials, expect $300K-$3M+ in clinical costs alone.
Step 4: Regulatory Precedent Review
Research how FDA treated similar devices:
Recent clearances: Check 510(k) database for devices cleared in last 24 months
FDA guidance: Look for device-specific guidance documents
Warning letters: Search FDA warning letters for compliance issues in your device category
Recalls: Check MAUDE database for safety issues with similar devices
💡 Complizen Advantage:
Complizen consolidates these data sources — 510(k)s, MAUDE, recalls, and warning letters — into a single dashboard so you see the full regulatory landscape for your device type.
Step 5: Feasibility Decision
Based on your assessment, determine if your device is:
✅ Regulatory viable: Clear pathway exists, reasonable cost/timeline, precedent supports clearance
⚠️ Regulatory challenging: Pathway unclear, high clinical burden, limited precedent
❌ Regulatory non-viable: No pathway available, prohibitive costs, FDA concerns documented
Stage 2: Pathway Evaluation and Selection
Choosing the right regulatory pathway is the most consequential strategic decision you'll make. Get it right and you'll reach market in 12-18 months. Get it wrong and you'll waste 6-12 months resubmitting through a different pathway.
What Are My Regulatory Pathway Options?
The FDA offers three primary pathways for medical device market entry, each with different requirements, timelines, and costs.
Best for: Class II devices with suitable predicate devices
Timeline: 3-12 months from submission to clearance
Cost: $50K-$200K+ (testing, consultant fees, FDA user fees)
Requirements:
Demonstrate substantial equivalence to legally marketed predicate device
Provide performance testing data (bench testing, biocompatibility, electrical safety)
Typically no clinical data required (unless predicate required it)
eSTAR formatted submission
Success rate: Approximately 85-90% of 510(k)s are cleared (after potential Additional Information requests)
💡 Complizen Advantage: Compare hundreds of predicate 510(k)s by intended use and testing type in seconds using Complizen’s Predicate Intelligence. It flags which tests and standards each predicate used so you know exactly how to prepare your own submission.
Best for: Novel Class I or II devices without suitable predicates
Timeline: 6-12 months from submission to authorization
Cost: $75K-$300K+ depending on special controls and clinical data requirements
Requirements:
Demonstrate device is low-to-moderate risk
Propose special controls (performance standards, labeling, post-market surveillance)
May require limited clinical data depending on device
Your device becomes new predicate for future 510(k)s
Success rate: Approximately 60-70% of De Novo requests are granted
Best for: Class III devices that support/sustain life or present significant risk
Timeline: 1-3 years from submission to approval
Cost: $500K-$5M+ (clinical trials dominate costs)
Requirements:
Extensive clinical trials proving safety and effectiveness
Comprehensive manufacturing information
Advisory Committee review (for most novel devices)
Post-approval studies often required
Ongoing PMA supplements for any modifications
Success rate: Approximately 40-50% of original PMAs are approved on first submission
How Do I Choose the Right Pathway?
Use this decision framework to evaluate pathway options systematically.
Decision Framework: Pathway Selection Matrix
Question 1: What is my device classification?
Class I → Most are exempt (no premarket submission)
Class II → Usually 510(k) or De Novo
Class III → PMA required (or HDE for rare diseases)
Question 2: Does a suitable predicate device exist?
✅ YES → Evaluate 510(k) pathway
Same intended use as your device?
Similar technological characteristics?
Currently marketed (not recalled)?
Strong substantial equivalence argument possible?
❌ NO → Evaluate De Novo pathway (if Class I/II) or PMA (if Class III)
Question 3: Do technological differences raise new safety questions?
✅ YES → De Novo or PMA likely required
❌ NO → 510(k) pathway viable
Question 4: What clinical data do I have or can I generate?
Bench testing only → 510(k) pathway
Limited clinical data → De Novo pathway possible
Extensive clinical trials → PMA pathway (or required for 510(k) if predicate had trials)
Question 5: What timeline and budget constraints do I have?
12-18 months, $500K budget → Must pursue 510(k)
18-30 months, $2M budget → De Novo viable
3-5 years, $5M+ budget → PMA viable
Still uncertain? Request an FDA Pre-Submission (Q-Sub) meeting for pathway guidance. The FDA will provide written feedback on your proposed pathway within 75 days.
Should I Consider Alternative Pathways?
Beyond the three primary pathways, evaluate these alternatives for specific situations:
Best for: Devices treating life-threatening conditions with significant advantages over existing alternatives
Benefits:
Expedited FDA review and priority processing
More frequent FDA interactions and feedback
Potential for expedited Medicare reimbursement
Considerations: Requires preliminary clinical evidence and commitment to frequent FDA engagement
Best for: Devices treating rare diseases affecting <8,000 U.S. patients annually
Benefits:
Less rigorous clinical requirements than PMA (demonstrate probable benefit vs. effectiveness)
Lower FDA user fees
Faster approval timeline
Considerations: Significant market size limitations, restricted to humanitarian use
Stage 3: Resource Planning and Team Strategy
Regulatory success requires the right team, appropriate expertise, and realistic budget allocation. Under-resourcing regulatory activities is the fastest way to blow timelines and budgets.
What Regulatory Resources Do I Need?
In-House vs. Consultant Strategy
Most companies face the consultant decision early: build internal regulatory capability or hire external expertise. The optimal answer depends on your device complexity, team experience, and long-term strategy.
Regulatory Consultant Advantages:
✅ FDA experience: Know exactly what FDA expects, how to structure submissions, common pitfalls
✅ Faster timeline: Avoid learning curve and prevent mistakes that trigger RTA holds
✅ Reduced risk: Consultants prevent the administrative deficiencies that derail 60% of first submissions
✅ Cost predictability: Fixed-fee projects provide budget certainty
Consultant Costs:
510(k) submission: $30K-$150K depending on complexity
De Novo submission: $50K-$200K
PMA submission: $200K-$500K+
Hourly rates: $75-$400/hour depending on expertise level
In-House Regulatory Team Advantages:
✅ Long-term cost savings: No consultant fees for ongoing submissions
✅ Institutional knowledge: Build regulatory expertise for future products
✅ Direct FDA relationships: Your team becomes FDA's primary contact
✅ Faster iterations: In-house team responds immediately to questions
In-House Costs:
Regulatory Affairs Manager: $90K-$150K annually + benefits
VP Regulatory Affairs: $150K-$250K+ annually + benefits
Supporting staff: $60K-$90K per person annually
Decision Framework: Consultant vs. In-House
✅ Hire consultant if:
This is your first FDA submission
Your device is PMA or complex De Novo
Timeline is critical (funding runway, market window)
Team lacks FDA regulatory experience
You need to minimize RTA/AI response risk
💰 Build in-house if:
You have pipeline of multiple products
You're building long-term regulatory capabilities
You have experienced regulatory staff available
Budget constraints prohibit consultant fees
Your device is straightforward 510(k) with clear predicate
Hybrid approach: Many successful companies hire consultants for first submission, then bring regulatory expertise in-house for modifications and future products. This balances speed, cost, and capability building.
💡 Complizen Advantage:
Complizen’s Regulatory Strategy Workspace automates the groundwork — classification, predicate mapping, and testing standards — reducing consultant research hours (typically $10 K – $30 K) to mere hours of platform-guided analysis.
Stage 4: Timeline and Milestone Planning
Regulatory timelines determine your entire business strategy: when you need funding, when you can generate revenue, and when you'll face competitive threats.
How Long Does Each Pathway Really Take?
Understanding realistic timelines—not FDA's idealized review clocks—helps you plan development and fundraising strategically.
510(k) Pathway Timeline (12-24 months total)
Months 1-8: Development & Testing
Design and development: 4-6 months
Design controls implementation: Ongoing
Performance testing: 2-4 months
Biocompatibility testing: 3-4 months
Electrical safety testing: 2-3 months
Months 6-10: Pre-Submission Preparation
QMS implementation: 4-6 months
Design History File compilation: 2-3 months
Technical file assembly: 1-2 months
510(k) drafting: 2-4 months
Internal review: 2-4 weeks
Months 10-14: FDA Review
Submission to RTA decision: 15 days
FDA substantive review: 90 days (FDA clock)
Additional Information requests: 30-90 days (if needed)
Final clearance: 2-4 weeks after AI response
Months 14-16: Post-Clearance
Manufacturing scale-up: 2-4 months
Labeling finalization: 1-2 months
Launch preparation: 1-2 months
Reality check: FDA's 90-day review clock doesn't include Additional Information response time. Most 510(k)s receive at least one AI request, extending actual timeline to 6-12 months from submission to clearance.
De Novo Pathway Timeline (18-30 months total)
Months 1-10: Development & Testing
Design and development: 6-8 months
Performance testing: 3-4 months
Limited clinical data collection: 4-6 months (if required)
Special controls development: 2-3 months
Months 8-14: Pre-Submission Strategy
Pre-Sub meeting with FDA: 2-4 months
QMS implementation: 4-6 months
De Novo request preparation: 3-5 months
Months 14-22: FDA Review
Submission to FDA: Month 14
FDA review: 150 days (FDA clock)
Interactive review cycles: 2-4 months (typical)
Final authorization: 1-2 months
Months 22-26: Post-Authorization
Manufacturing scale-up: 2-4 months
Market launch: 2-3 months
PMA Pathway Timeline (3-5 years total)
Year 1: Preclinical Development
Device design and optimization: 6-8 months
Preclinical testing (animal studies): 4-6 months
Manufacturing process development: 6-12 months
Months 12-18: Clinical Trial Preparation
IDE submission and approval: 3-6 months
Clinical site selection and contracts: 2-4 months
IRB approvals: 2-4 months
Months 18-36: Clinical Trials
Patient enrollment: 12-18 months
Data collection and monitoring: 12-24 months
Data analysis: 3-6 months
Months 36-42: PMA Preparation
Clinical data analysis: 3-4 months
PMA application compilation: 4-6 months
Internal review and revision: 2-3 months
Months 42-54: FDA Review
FDA filing decision: 45 days
FDA substantive review: 180 days (FDA clock)
Advisory Committee meeting: 2-4 months preparation
Facility inspection: 1-2 months
Final approval: 2-4 months
Year 5+: Post-Approval
Manufacturing scale-up: 6-12 months
Commercial launch: 3-6 months
What Are Critical Path Activities?
Critical path activities are tasks that directly impact your timeline—delays in these activities delay your entire project. Identify and prioritize them ruthlessly.
510(k) Critical Path:
Biocompatibility testing (3-4 months) - Start during design phase, longest lead time
Predicate device selection (2-4 weeks) - Wrong choice forces complete restart
Performance testing (2-4 months) - Can't draft submission without results
Substantial equivalence argument (2-4 weeks) - Core of your 510(k)
eSTAR formatting (1-2 weeks) - Administrative errors trigger RTA
💡 Complizen Advantage:
Complizen’s Predicate Intelligence compresses 4–6 weeks of manual research into hours by surfacing predicate 510(k)s and their testing strategies instantly.
PMA Critical Path:
IDE approval (3-6 months) - Can't start clinical trials without it
Patient enrollment (12-18 months) - Often the longest single activity
Clinical data collection (12-24 months) - Sequential with enrollment
Advisory Committee preparation (2-4 months) - High-stakes presentation
Facility inspection (1-2 months) - Can delay approval if deficiencies found
Timeline Optimization Strategies:
✅ Parallelize activities: Begin QMS implementation during testing phase
✅ Start testing early: Long lead time tests (biocompatibility) during design
✅ Engage FDA proactively: Pre-Sub meetings prevent late-stage surprises
✅ Use established test labs: FDA-recognized labs reduce questions
✅ Prepare for AI requests: Draft responses to anticipated FDA questions in advance
Stage 5: Multi-Market Strategy Considerations
Most medical device companies target multiple geographic markets. Your regulatory strategy should address market entry sequencing: US first, EU first, or simultaneous pursuit.
U.S.–First Strategy (FDA → CE Mark)
Advantages
Largest single market
Global credibility: FDA clearance validates worldwide adoption
Single authority: One submission vs. multiple EU notified bodies
Investor preference: U.S. VCs prioritize FDA milestones
Disadvantages
Longer total timeline (esp. PMA 1–3 yr)
Higher costs (user fees + testing + clinical)
Revenue delay until FDA clearance
Best for
Devices targeting primarily U.S. patients
VC-backed startups seeking FDA signal
Breakthrough / high-risk devices where FDA validation adds moat
EU–First Strategy (CE Mark → FDA)
Advantages
Faster time to market: Often 6–12 month ahead of FDA
Earlier revenue: EU sales can fund U.S. submission
Clinical leverage: EU real-world data supports FDA review
Lower initial costs: CE mark cheaper than PMA
Disadvantages
Fragmented market: 27 systems, languages, reimbursements
Notified-body backlog: MDR capacity still limited
Lower global prestige: FDA clearance remains gold standard
Regulatory uncertainty: MDR rules continue to evolve
Best for
Companies with limited funding needing cash flow
Devices requiring EU clinical data before FDA
Firms already operating in Europe
Simultaneous Strategy (FDA + CE Mark)
Advantages
Fastest global entry: Dual launch for maximum reach
Competitive edge: Beat rivals in both markets
Efficiency: Shared testing and design control data
Disadvantages
Resource-intensive: ≈ 1.5 – 2× staff and budget
Complex coordination: Different formats and timelines
Risk concentration: Delay in one regulator affects both
Best for
Well-funded teams (>$5 M) with mature QMS
Clear regulatory path in both regions
Competitive markets where speed is critical
Stage 6: Risk Identification and Mitigation
Every regulatory strategy has risks that could derail your timeline, budget, or market entry. Identify them early and build mitigation plans.
What Are the Biggest Regulatory Risks?
Risk 1: Wrong Pathway Selection
Impact: 6-12 months wasted, $50K-$200K spent on wrong submission approach
Mitigation strategies:
✅ Conduct thorough predicate analysis before committing to 510(k)
✅ Request Pre-Sub meeting if pathway is uncertain
✅ Engage regulatory consultant for pathway validation
✅ Review recent FDA clearances for similar devices
Risk 2: Inadequate Testing Strategy
Impact: Additional Information requests, 3-6 months delay, $50K-$150K additional testing costs
Mitigation strategies:
✅ Review predicate testing strategies and FDA standards
✅ Use FDA-recognized test labs for critical testing
✅ Build testing margin (exceed minimum requirements)
✅ Request Pre-Sub feedback on testing protocols
Risk 3: RTA Hold (Refuse to Accept)
Impact: 30-60 day delay, administrative embarrassment, potential consultant fees for resubmission
Mitigation strategies:
✅ Use current eSTAR template precisely
✅ Include all required sections (even if "Not Applicable")
✅ Have third party review submission before filing
✅ Verify all administrative requirements (user fees, signatures, dates)
Risk 4: Clinical Data Deficiencies
Impact: 6-18 months delay, $200K-$2M+ additional clinical costs, potential pathway change
Mitigation strategies:
✅ Engage FDA early with clinical protocol review
✅ Use FDA-recognized endpoints and study design
✅ Enroll adequate patient numbers with margin
✅ Conduct interim analyses to identify issues early
Risk 5: Funding Shortfall Mid-Submission
Impact: Forced to pause submission, lose momentum, potentially lose FDA reviewer assignment
Mitigation strategies:
✅ Budget 1.5-2x initial regulatory estimate
✅ Secure funding before starting expensive clinical trials
✅ Maintain 12-18 months runway beyond expected clearance
✅ Have bridge funding sources identified
Risk 6: Competitor Predicate Device Recall
Impact: If using recalled device as predicate, must find new predicate or change pathway
Mitigation strategies:
✅ Choose predicates with strong safety records
✅ Review MAUDE database for predicate safety issues
✅ Identify backup predicate devices
✅ Monitor FDA recall notices throughout development
💡 Complizen Advantage: Complizen monitors MAUDE adverse events and recalls in real time, flagging predicate risk before it affects your submission.
Risk 7: Design Changes During Development
Impact: Testing invalidation, design control gaps, submission delays
Mitigation strategies:
✅ Implement design controls from day one
✅ Use formal change control process
✅ Assess regulatory impact of every design change
✅ Maintain Design History File continuously
Risk 8: Key Personnel Departure
Impact: Institutional knowledge loss, timeline delays, submission quality issues
Mitigation strategies:
✅ Document regulatory decisions and rationale
✅ Use consultants as continuity backup
✅ Cross-train team on regulatory requirements
✅ Maintain Design History File meticulously
Common Strategic Mistakes That Delay Market Entry
Mistake #1: Treating Regulatory as Implementation Phase (Not Strategic Planning)
Most companies treat regulatory as something that happens after development: "We'll figure out FDA when the product is ready." This approach leads to design changes, wasted testing, and blown timelines.
The cost: Companies that plan regulatory during concept phase reach market 6-12 months faster than companies that retrofit regulatory compliance.
How to avoid: Integrate regulatory requirements into product requirements from day one. Your product spec should include FDA classification, applicable standards, and testing requirements—not just technical features.
Mistake #2: Optimistic Timeline and Budget Assumptions
First-time founders consistently underestimate regulatory timelines by 50-70% and budgets by 100-200%. This creates funding gaps mid-submission and forces unfavorable financing.
The cost: Running out of money during FDA review forces bridge financing at terrible terms or submission withdrawal.
How to avoid: Use realistic timelines based on actual FDA data (not FDA's idealized review clocks). Budget 1.5-2x your initial estimate. Assume you'll receive Additional Information requests.
Mistake #3: DIY Approach Without Regulatory Expertise
Founders with engineering backgrounds often believe they can "figure out" FDA regulations through research. While possible for simple 510(k)s, this approach triggers RTA holds and submission deficiencies.
The cost: RTA holds delay review by 30-60 days. Multiple AI request cycles add 3-6 months. Design control gaps create warning letter risk.
How to avoid: Hire experienced consultant for first submission—even if planning to build in-house capability later. The learning curve is expensive; buy expertise for your first product.
Mistake #4: Wrong Predicate Selection
Choosing a predicate device that's too different technologically or has substantive differences in intended use creates an impossible substantial equivalence argument.
The cost: Wrong predicate forces submission withdrawal and new pathway selection—wasting 6-12 months and $50K-$150K.
How to avoid: Validate predicate selection through Pre-Sub meeting. Review predicate's 510(k) summary thoroughly. Confirm predicate is currently marketed and has no safety issues.
💡 Complizen Advantage: Complizen’s Predicate Intelligence instantly compares your device’s intended use and risk profile against thousands of 510(k)s—flagging unsuitable predicates before submission.
Mistake #5: Starting Testing Too Late
Most companies wait until design is "frozen" to begin formal testing. But many tests take 3-4 months, and failures require design changes and retesting.
The cost: Sequential testing extends timelines by 6-12 months and increases costs as design iterations require new rounds of testing.
How to avoid: Begin testing during design phase on design iterations. Use early testing to inform design decisions. Plan for test failures and build iteration time into timeline.
Mistake #6: Ignoring Post-Clearance Requirements
Companies focus entirely on "getting to clearance" and neglect QMS implementation, post-market surveillance planning, and ongoing compliance requirements.
The cost: FDA inspections within 2 years of clearance reveal QMS deficiencies, triggering warning letters or consent decrees that halt manufacturing.
How to avoid: Build QMS during development phase, not after clearance. Plan for post-market costs in your budget. Hire quality/regulatory staff before launch, not after.
Mistake #7: No Contingency Planning
Most regulatory roadmaps show the "happy path" with no consideration of what happens when things go wrong—and things always go wrong.
The cost: When unexpected issues arise (RTA hold, test failures, Additional Information requests), teams scramble reactively instead of executing predetermined plans.
How to avoid: Build contingency scenarios into your roadmap. Identify backup predicates. Plan response strategies for likely FDA questions. Maintain budget contingency of 30-50%.
Complizen’s Regulatory Strategy Builder
Building your FDA strategy shouldn’t take months of guesswork and spreadsheet chaos.
Maps your pathway instantly: 510(k), De Novo, or PMA — backed by real FDA data.
Analyzes predicates automatically: surfaces comparable devices, summaries, and testing methods in seconds.
Recommends recognized standards: links each test requirement to official FDA or ISO references.
Builds your submission roadmap: outlines every document, test, and milestone based on your device’s risk profile.
🚀 Why It Matters
Cut weeks of database research into minutes.
Reduce RTA risk with complete, source-linked documentation.
Align your submission with how the U.S. FDA actually reviews devices today.
Present investors with a clear, defensible regulatory timeline and budget.
💡 Designed For
Startups preparing their first FDA submission.
Consulting firms managing multiple client devices.
Established manufacturers optimizing ongoing compliance workflows.
Complizen transforms regulatory planning from a guessing game into a repeatable, transparent process — built on real FDA data, not opinions.
👉 Start free at complizen.ai
FAQ: Medical Device Regulatory Strategy
When should I start building my regulatory strategy?
Start during concept phase—before design decisions or testing begins. Companies that integrate regulatory from day one reach market 6-12 months faster than those who retrofit compliance after development.
Do I need a regulatory consultant for my first FDA submission?
Strongly recommended for first-time submitters. Consultants prevent RTA holds (affecting 60% of first submissions), avoid expensive mistakes, and typically accelerate timelines by 3-6 months despite their cost.
How much should I budget for regulatory activities?
510(k): $50K-$200K+. De Novo: $75K-$300K+. PMA: $500K-$5M+. Budget 1.5-2x your initial estimate as most startups underestimate costs by 100-200%, creating funding gaps mid-submission.
Should I pursue FDA clearance or CE marking first?
FDA-first for US-focused companies, VC-backed startups, and breakthrough devices. CE-first for companies needing early revenue or devices requiring clinical data.
What's the difference between regulatory strategy and regulatory submission?
Strategy is planning (pathway selection, resources, timeline, risk mitigation) done during concept phase. Submission is execution (preparing documentation, compiling data) done after testing completion.
How do I know if my predicate device is suitable for 510(k)?
Suitable predicates have same intended use, similar technological characteristics, currently marketed status, and no major safety issues. Validate through FDA Pre-Sub if uncertain—wrong predicate wastes 6-12 months.
What happens if FDA disagrees with my regulatory pathway?
FDA may issue "Not Substantially Equivalent" or refuse your pathway. Options: withdraw and resubmit through correct pathway, request supervisory review, or provide additional data. Pre-Sub meetings prevent this scenario.
How long does it really take to get FDA clearance?
510(k): 12-24 months total. De Novo: 18-30 months. PMA: 3-5 years. These include development, testing, and FDA review—not just FDA's 90-day or 180-day review clock.
Can I change my regulatory strategy mid-development?
Yes, but expensive. Pathway changes cost $50K-$200K+ depending on progress. Prevention: validate pathway early through Pre-Sub meeting and conduct thorough feasibility assessment before committing.
What regulatory strategy mistakes are most expensive?
Wrong pathway selection (6-12 months, $50K-$200K wasted), inadequate testing (3-6 months delay, $50K-$150K extra), RTA holds (30-60 days), funding shortfalls mid-submission, and ignoring post-clearance requirements.
How do I evaluate regulatory consultants?
Evaluate based on: FDA experience in your device category, recent clearances (ask for references), pathway expertise (510(k), De Novo, PMA), technology understanding, and transparent pricing. Red flags: clearance guarantees or vague pricing.



