How to Bring a Medical Device to the U.S. Market: Complete 2025 Guide
- Nov 9, 2025
- 13 min read
To bring a medical device to the U.S. market: (1) Classify your device (Class I, II, or III), (2) select your regulatory pathway (510(k), De Novo, or PMA), (3) complete required testing, (4) prepare and submit your FDA application, and (5) maintain post-clearance QMS compliance. Timeline ranges from 3-6 months for 510(k) to 1-3 years for PMA.
This guide provides the complete roadmap from concept to U.S. market launch, with decision frameworks at each stage to help you avoid the expensive mistakes that derail 60% of first-time submissions. Whether you're a startup founder planning your first FDA submission or an international company entering the U.S. market, you'll learn exactly what happens when, what it costs, and which decisions determine success or failure.

What Makes U.S. Medical Device Market Entry Complex?
The global medical device market represents $671.49 billion by 2027, making it the world's largest and most lucrative market for medical technology. But this opportunity comes with regulatory complexity that catches most companies off guard.
Unlike many international markets where you simply demonstrate safety and performance, the FDA requires you to prove substantial equivalence to existing devices (for 510(k)) or provide comprehensive clinical data demonstrating safety and effectiveness (for PMA). The classification of your device—determined by its intended use and risk level—dictates your entire regulatory strategy, timeline, and budget.
And the story doesn’t end at clearance. Many B2B medical-device decision-makers conduct extensive online research before ever engaging a sales rep, so achieving regulatory clearance is just the first step in capturing market traction.
The 5-Stage Roadmap to U.S. Market Entry
Every medical device follows this fundamental journey to the U.S. market, though timelines and complexity vary dramatically based on classification and pathway. Here's the complete roadmap with decision points that determine your success.
Stage 1: Pre-Market Preparation (≈ Months 1–6)
What Is Medical Device Classification and Why Does It Matter?
Medical-device classification drives everything — your regulatory pathway, required testing, budget, and time-to-market. The FDA categorizes devices by intended use and risk level under 21 CFR Parts 862-892.
Class I (low risk) – e.g., tongue depressors, elastic bandages, exam gloves. Most are exempt from 510(k); only registration + listing required. Typical timeline: 1–2 months | Typical cost: $5 K–$15 K.
Class II (moderate risk) – e.g., powered wheelchairs, infusion pumps, surgical drapes. Usually require 510(k) clearance demonstrating substantial equivalence. Timeline: 3–12 months | Cost: $50 K–$200 K +.
Class III (high risk) – e.g., pacemakers, heart valves, implantable defibrillators. Require PMA supported by extensive clinical data. Timeline: 1–3 years | Cost: $500 K–$5 M +.
Two devices with similar technology may fall into different classes depending on intended use or patient contact.
Decision Framework – How to Classify Your Device
Search FDA’s Product Classification Database.
Review the applicable regulation number (21 CFR Part).
Determine if it’s a combination product (drug/device or biologic/device).
For novel technologies, consider an FDA Q-Submission to discuss classification early.
SO WHAT: Misclassification can derail your submission, waste months, and force a restart. It’s the single most critical early decision.
How to Develop a Testing Strategy Before FDA Submission
Your testing must prove the device performs as intended and meets FDA-recognized standards.
Performance Testing: mechanical, electrical, software validation, and shelf-life or stability testing per FDA-recognized standards.
Biocompatibility Testing: follow ISO 10993-1 (2018) for cytotoxicity, sensitization, irritation, and systemic toxicity.
Clinical Testing:
Sterilization Validation: use FDA-recognized standards such as ISO 11135 (EtO) or ISO 11137 (radiation).
SO WHAT: Delaying test plans is the #1 cause of submission delays. Start verification and validation during design — not after freeze.
What Are Design Controls and When Do I Need Them?
Under 21 CFR 820.30, design controls apply to all Class II and III devices.
Key phases include: Design & Development Planning → Design Input → Design Output → Design Review → Verification → Validation → Transfer → Change Control.
Maintain a Design History File (DHF) documenting every activity; FDA inspectors routinely review DHFs during audits and premarket evaluations.
SO WHAT: Inadequate design controls are among the top FDA 483 observations each year. Building compliance from day one is cheaper and faster than fixing it later.
Stage 2 – Regulatory Pathway Selection (≈ Months 3 – 8)
What Is the 510(k) Pathway and When Should You Use It?
The 510(k) pathway—named after Section 510(k) of the FD&C Act—lets manufacturers market most Class II and certain Class I devices by proving substantial equivalence to a legally marketed predicate device. Roughly 80–85 % of U.S. medical-device submissions follow this route.
Substantial equivalence means your device has the same intended use and technological characteristics as the predicate—or differences that don’t raise new safety or effectiveness questions.
510(k) Timelines:
Straightforward devices: ≈ 3–6 months
Complex devices: ≈ 6–12 months (including Additional Information cycles)
FDA’s review clock is 90 days, but most submissions receive at least one AI request that extends the timeline.
510(k) Costs (2025): ≈ $50 k–$200 k+ total (including testing and consultant fees) plus FDA user fee $26,067 standard / $6,517 small business.
Types of 510(k):
Traditional: Standard predicate comparison.
Special: For modifications to your own cleared device.
Abbreviated: Relies on FDA guidances or recognized standards.
Decision Framework – Can You Use 510(k)?
✅ YES if device is Class I or II and predicate exists.
❌ NO if no predicate (consider De Novo) or device is Class III (PMA).
SO WHAT: The 510(k) pathway is fast and affordable only if you choose the right predicate and build a strong substantial-equivalence argument from day one.
What Is the De Novo Pathway and How Does It Work?
The De Novo pathway establishes a new classification for novel low-to-moderate risk devices without a predicate. It’s the FDA’s innovation route for emerging technologies.
Timeline: ≈ 6–12 months (total); 150-day FDA goal often extended with AI requests.
Cost Range: ≈ $75 k–$300 k+ depending on complexity and need for clinical data.
When a De Novo is granted, your device creates a new predicate that you and competitors can reference for future 510(k)s — a strategic first-mover advantage.
Special Controls (specified performance standards, labeling, post-market requirements) are defined jointly with FDA during the review.
Decision Framework – Should You Pursue De Novo?
✅ YES if device is novel, low-to-moderate risk, and you want to create a new predicate.
❌ NO if predicate exists or timeline pressure is critical.
SO WHAT: De Novo is the innovation pathway — more work than 510(k), but far faster and cheaper than PMA.
What Is the PMA Pathway and Which Devices Require It?
Premarket Approval (PMA) is the FDA’s most stringent process, required for Class III devices that support or sustain life or present significant risk.
Timeline: ≈ 1–3 years (180-day FDA review clock often extended for AI and Advisory Committee review).
Costs (2025): ≈ $500 k–$5 M+ including clinical trials and consultants plus FDA user fee $579,272 standard / $144,818 small business.
A complete PMA includes clinical trial data (often under IDE), manufacturing process details, bench and animal testing, proposed labeling, and sometimes a panel review.
Alternative Pathways to Explore:
Humanitarian Device Exemption (HDE): for conditions affecting < 8,000 patients per year.
Breakthrough Device Designation: for technologies addressing unmet needs with expedited review.
Product Development Protocol (PDP): rarely used PMA alternative for predictable technologies.
SO WHAT: PMA is costly and slow, but it proves your device meets the highest safety and performance standards — a major credibility advantage with clinicians and investors.
Stage 3 – Pre-Submission Strategy (≈ Months 6 – 12)
What Is an FDA Pre-Submission (Q-Submission) and Should You Request One?
An FDA Pre-Submission (Pre-Sub)—part of the Q-Submission (Q-Sub) program—lets you formally obtain FDA feedback before submitting your 510(k), De Novo, or PMA. It’s one of the most under-used strategic tools in U.S. regulatory planning.
Through a Q-Sub, you can:
Get FDA input on your testing strategy and study design
Confirm your predicate device selection
Discuss clinical trial protocols
Clarify regulatory pathway or classification questions
Validate your substantial-equivalence argument
A well-timed Q-Sub can save six months or more by preventing costly missteps before investing in testing or clinical trials.
Q-Submission
Timeline: FDA aims to provide feedback within 75 days of receipt (written or meeting).
Costs: Typically $5 000 – $20 000 for preparation if using consultants.
There is no FDA user fee for most Q-Sub types.
Decision Framework – When to Request a Pre-Sub✅ Request if:
Your device is novel or first-in-class
You’re uncertain about classification or pathway
Your testing strategy is complex or expensive
You plan to conduct clinical trials
You’re using new technology or a novel predicate
❌ Skip if:
Your 510(k) has a well-defined predicate and routine tests
Similar devices were recently cleared
Your regulatory strategy is already validated
SO WHAT: Companies that engage FDA early move faster. Pre-Sub meetings reduce uncertainty, minimize review cycles, and prevent expensive rework.
How Do I Choose Between Hiring a Consultant vs. Going Direct?
Most medical device companies eventually face this decision: hire a regulatory consultant or manage the FDA process in-house. Neither path is universally right — it depends on your team’s experience, device complexity, and timeline pressure.
Regulatory Consultant Advantages
Experience with FDA: Consultants know how reviewers think, how to structure submissions, and which pitfalls trigger Refuse-to-Accept (RTA) holds.
Faster timelines: You bypass the learning curve and avoid preventable rejections.
Reduced RTA risk: Roughly 30–40% of first-time 510(k)s encounter RTA issues — experienced consultants help prevent this.
Bandwidth: Your engineers focus on product development, not FDA paperwork.
Consultant Costs: $75–$300/hour (independent consultants); $150–$400/hour (consulting firms)
Average total: $30K–$150K for a 510(k), $200K–$500K+ for a PMA.
In-House Approach Advantages
Cost savings: No external consulting fees.
Knowledge building: You develop lasting in-house regulatory expertise.
Direct FDA relationship: You become your company’s voice to FDA reviewers.
Challenges:
Steep learning curve — first submissions take longer.
Higher chance of RTA due to administrative errors.
Opportunity cost — your core team spends time learning FDA protocols instead of advancing the product.
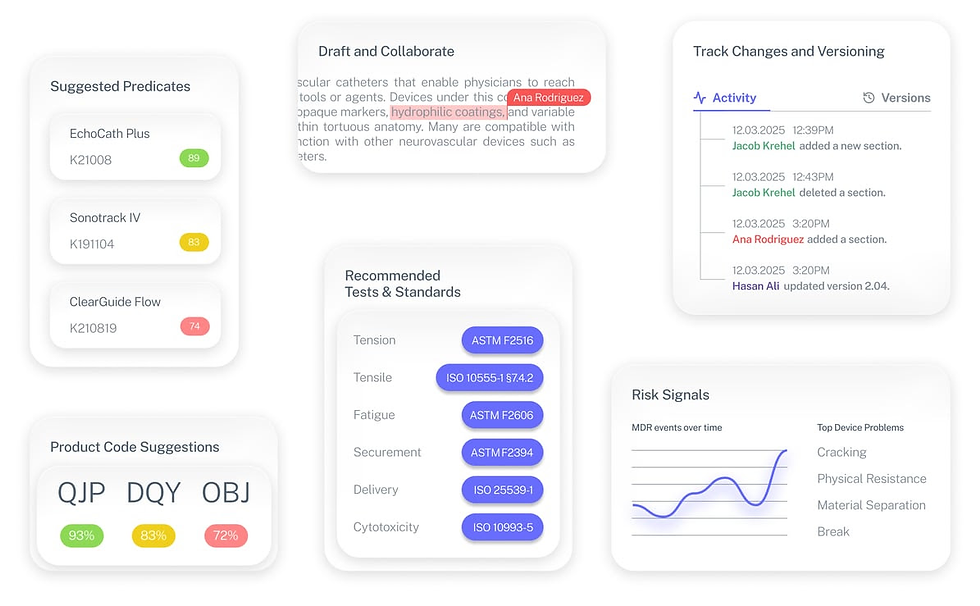
🧩 Where Complizen Helps: For teams going direct, Complizen acts as your regulatory co-pilot. It guides you step-by-step through classification, predicate analysis, test selection, and submission prep, referencing actual FDA sources. What once took weeks of scattered research now takes minutes, even without a full-time consultant.
SO WHAT: The consultant decision isn’t purely about cost — it’s about risk mitigation and timeline optimization. Most first-time manufacturers actually save money by pairing expert guidance with Complizen’s intelligent FDA workspace, avoiding the most expensive delay of all: starting over.
Stage 4: Submission and Review (Months 10-18)
How Do I Prepare My FDA Submission Using eSTAR?
The FDA requires electronic submissions through the Electronic Submission Template and Resource (eSTAR) system. Understanding eSTAR formatting requirements is critical—administrative deficiencies cause most Refuse to Accept (RTA) holds.
Each section has specific formatting requirements. Missing required information, incorrect file formats, or improper organization triggers an RTA hold—delaying your review by 30-60+ days while you resubmit.
SO WHAT: RTA holds delay your review by 30-60+ days. Invest time in proper eSTAR formatting—it's not glamorous, but it prevents expensive delays.
What Happens During FDA Review?
Once your submission is accepted, the FDA review clock begins. Understanding this process helps you prepare for what's coming and respond quickly to FDA requests.
510(k) Review Process (90 days):
Day 1-15: Administrative screening (RTA decision)
Day 15-75: Substantive review by FDA reviewer
Day 75-90: Additional Information requests (if needed), FDA decision
Common Additional Information requests:
Clarification of substantial equivalence claims
Additional testing data or protocols
Labeling revisions
Software documentation
Biocompatibility testing details
How to handle AI requests:
Respond within 180 days (or your submission is withdrawn)
Answer every question completely (partial responses trigger additional AI requests)
Use the exact question numbering from FDA's letter
Provide supporting documentation for all claims
Consider requesting a teleconference if questions are unclear
PMA Review Process (180 days):
Day 1-45: Administrative filing decision
Day 45-135: Substantive review, possible facility inspection
Day 135-165: Advisory Committee meeting (for novel devices)
Day 165-180: FDA approval decision
SO WHAT: The review process isn't passive waiting. Companies that respond quickly and completely to FDA questions get cleared faster—often 2-3 months faster than companies that provide incomplete responses.
What Is an RTA Hold and How Do I Avoid It?
A Refuse to Accept (RTA) hold means the FDA refuses to begin substantive review of your submission due to administrative deficiencies. This is the most common and most preventable submission failure.
60% of submissions receive RTA holds or Additional Information requests, primarily due to administrative issues, not technical problems.
Common RTA triggers:
Missing required sections in eSTAR format
Incomplete device description
Missing or incorrect user fees
Inadequate labeling information
Poor organization or missing table of contents
Missing truthful and accuracy statement
The RTA process:
FDA issues RTA letter (within 15 days of receipt)
You have 180 days to resubmit
New review clock starts after resubmission
You've lost 30-60+ days minimum
RTA Prevention Checklist:
✅ Use current eSTAR template
✅ Include all required sections (even if "Not Applicable")
✅ Verify user fee payment and confirmation number
✅ Complete device description with photos/diagrams
✅ Include all required labeling (final or mock-up)
✅ Verify predicate device 510(k) numbers are accurate
✅ Include executive summary and table of contents
✅ Have third party review submission before filing
SO WHAT: RTA holds are administrative failures, not technical failures. They're completely preventable with proper submission preparation—yet they delay most first-time submissions.
Stage 5: Post-Clearance Requirements (Month 18+)
What QMS Requirements Apply After FDA Clearance?
FDA clearance isn't the finish line—it's the starting line for ongoing compliance obligations. The FDA's Quality System Regulation (QSR) under 21 CFR Part 820 governs how you manufacture, test, and distribute your device.
Key QMS requirements:
Design Controls: Maintain Design History File (DHF) for design changes
Document Controls: Procedures for document creation, review, approval, distribution
Purchasing Controls: Supplier qualification and component verification
Production and Process Controls: Manufacturing procedures, equipment validation
CAPA (Corrective and Preventive Action): System for addressing quality issues
Complaint Handling: Procedures for receiving and investigating complaints
MDR (Medical Device Reporting): Required reporting of adverse events
Labeling Controls: Ensuring labeling accuracy and traceability
The QMS requirement most companies underestimate: You must maintain your QMS from day one of marketing, not build it after your first FDA inspection.
When does FDA inspect your facility? Class II and III device manufacturers can expect FDA inspection within 2 years of first clearance. The FDA arrives unannounced for most routine inspections.
SO WHAT: FDA warning letters and consent decrees usually result from QMS failures, not device design failures. Build your QMS during development, not after clearance.
What Post-Market Surveillance Is Required?
Post-market surveillance includes all activities to monitor device performance after market launch. Requirements vary by device classification and specific FDA requirements.
Medical Device Reporting (MDR): Mandatory reporting of adverse events, malfunctions, and deaths within specific timeframes (5 days to 30 days depending on severity).
Post-Approval Studies: Some PMA approvals include requirements for post-approval clinical studies to gather additional long-term safety/effectiveness data.
Annual Registration and Listing: Update your FDA establishment registration and device listing annually (October 1 - December 31).
Periodic Reporting: PMA devices require periodic reports (annually or at intervals specified in approval order).
Post-Market Surveillance Studies: FDA may require specific studies for certain devices to monitor long-term safety or rare adverse events.
SO WHAT: Post-market compliance failures can result in consent decrees, product recalls, or revocation of clearance. Budget for ongoing regulatory operations, not just getting to market.
Common Mistakes That Derail U.S. Market Entry (and How to Avoid Them)
Mistake #1 — Choosing the Wrong Predicate Device
Selecting a predicate that differs in intended use or core technology makes a substantial-equivalence argument impossible. You’ll be forced to restart or pursue a De Novo, losing 6–12 months.
How to Avoid:
Research predicates in the FDA 510(k) database.
Verify they’re currently marketed and not recalled.
Use an FDA Pre-Submission to confirm your predicate strategy.
💡 Complizen Advantage: Complizen’s predicate-intelligence engine cross-references hundreds of cleared 510(k)s, surfacing the closest matches by intended use and technology so you start testing on solid ground.
Mistake #2 — Starting the FDA Process Too Late
Waiting until design freeze to consider regulatory strategy leads to costly redesigns and testing gaps.
How to Avoid:
Integrate FDA classification and testing strategy during concept phase.
Build design controls and documentation early.
Begin bench testing before verification.
💡 Complizen Advantage: Complizen maps your product concept to applicable product codes, predicates, and FDA standards within minutes — helping R&D and regulatory stay aligned from day one.
Mistake #3 — Underestimating QMS Requirements
FDA expects a compliant Quality Management System (QMS) before marketing, not after inspection. Delayed implementation leads to warning letters and consent decrees.
How to Avoid:
Implement QMS (21 CFR Part 820 → QMSR 2026) during development.
Train staff and document procedures as you create them.
Mistake #4 — Incomplete FDA Submission
Roughly one-third of 510(k)s face Refuse-to-Accept (RTA) holds due to missing sections, poor formatting, or outdated templates.
How to Avoid:
Use the latest eSTAR version.
Include every required section, even if marked “Not Applicable.”
Have an expert or automated checker review before filing.
Mistake #5 — Poor AI (Response) Strategy
Partial or vague replies to Additional Information (AI) letters stop your review clock and trigger new AIs.
How to Avoid:
Respond within 180 days with full documentation.
Follow FDA’s numbering exactly.
Request a teleconference for unclear questions.
Mistake #6 — Ignoring Post-Market Requirements
Clearance ≠ compliance. Neglecting MDR, registration renewal, or CAPA upkeep can halt manufacturing or trigger recalls.
How to Avoid:
Budget for ongoing regulatory operations.
Maintain complaint-handling and MDR procedures.
Audit your QMS routinely.
💡 Complizen Advantage: Complizen’s real-time monitoring pulls data from FDA recall and adverse-event databases, alerting you to potential field issues before they escalate.
Mistake #7 — Not Budgeting for Regulatory Reality
Many startups underestimate total regulatory spend — overlooking consultant fees, re-testing, or AI-response work.
How to Avoid:
Budget 1.5–2× your initial estimate.
Include contingency for testing, consultants, and post-market costs.
Plan a regulatory runway that extends beyond clearance.
The Fastest Path to Market
No more guesswork. Move from research to a defendable FDA strategy, faster. Backed by FDA sources. Teams report 12 hours saved weekly.
FDA Product Code Finder, find your code in minutes.
510(k) Predicate Intelligence, see likely predicates with 510(k) links.
Risk and Recalls, scan MAUDE and recall patterns.
FDA Tests and Standards, map required tests from your code.
Regulatory Strategy Workspace, pull it into a defendable plan.
👉 Start free at complizen.ai
FAQ: U.S. Medical Device Market Entry
How long does it take to get FDA clearance for a medical device?
Timeline depends on device classification and pathway: Class I exempt devices (1-2 months), 510(k) clearance (3-12 months), De Novo authorization (6-12 months), and PMA approval (1-3 years).
Can I market my device while waiting for FDA clearance?
No. Marketing a medical device in the U.S. without required FDA clearance or approval is prohibited and subjects you to warning letters, consent decrees, or criminal penalties. You can conduct limited pre-launch activities like market research, but cannot sell or distribute devices.
What happens if FDA refuses my 510(k)?
FDA issues a "Not Substantially Equivalent" (NSE) determination. You can withdraw and resubmit with additional data, request supervisory review, pursue De Novo pathway if device is low-moderate risk, or abandon U.S. market entry for that device design.
Do I need a U.S. facility to get FDA clearance?
No. International manufacturers can obtain FDA clearance using a U.S. Agent (FDA-required representative) and U.S. Designated Agent for service of process. However, you must comply with QSR requirements and FDA can inspect international facilities.
Can I make changes to my device after FDA clearance?
Yes, but changes may require new 510(k) submission depending on significance. Minor changes (e.g., labeling updates) may require letter to file. Major changes (intended use, technology, performance specifications) require new 510(k) or PMA supplement.
What is a U.S. Agent and do I need one?
A U.S. Agent is an FDA requirement for foreign manufacturers. The U.S. Agent must reside or maintain a business in U.S. and is responsible for FDA communications, device listing, and serving as emergency contact. Required for all foreign establishments.
How often does FDA inspect medical device facilities?
Class II and III manufacturers typically face FDA inspection within 2 years of first clearance, then every 2-4 years thereafter. High-risk or problem facilities may be inspected annually. Most routine inspections are unannounced.
What percentage of 510(k) submissions get RTA holds?
Approximately 60% of submissions receive RTA holds or Additional Information requests, primarily due to administrative deficiencies rather than technical issues. Proper eSTAR formatting and complete documentation reduce RTA risk significantly


