Pre-market Approval (PMA) Explained: The Complete 2025 Guide
- Jun 20, 2025
- 9 min read
Updated: Sep 7, 2025
Premarket Approval (PMA) is FDA’s most rigorous pathway, used for most Class III devices (those that support/sustain life, prevent major impairment, or pose potential unreasonable risk). A PMA must demonstrate reasonable assurance of safety and effectiveness with nonclinical and clinical evidence; FDA may conduct a manufacturing (QSR) inspection and sometimes an advisory-panel review.
Understanding PMA requirements early in development can save you years of delays and millions in development costs. This guide explains the PMA process in straightforward terms, helping you determine if your device needs PMA and what to expect from this demanding regulatory pathway.

What Is PMA (Pre-market Approval)? The Simple Answer
Pre-market Approval (PMA) is FDA's scientific review process for Class III medical devices—the highest-risk category of medical devices. Unlike 510(k) clearance, which relies on substantial equivalence to existing devices, PMA requires comprehensive clinical evidence proving your device is safe and effective for its intended use.
Think of PMA as FDA saying: "This device is so critical to patient safety that we need complete scientific proof it works as intended before allowing it on the market."
Why PMA Exists
FDA created PMA for devices that pose the highest risk to patients—typically life-sustaining, life-supporting, or implantable devices. These devices require the highest level of regulatory scrutiny because device failure could result in serious injury or death.
The PMA standard is "reasonable assurance of safety and effectiveness," which requires:
Comprehensive clinical data demonstrating device performance
Rigorous manufacturing controls ensuring consistent quality
Detailed risk-benefit analysis showing benefits outweigh risks
Post-market surveillance to monitor ongoing device performance
Which Devices Require PMA?
Most Class III medical devices require PMA approval before marketing. These are typically devices that support or sustain human life, are implanted in the body, or present unreasonable risk of illness or injury.
Examples of Devices That Typically Require PMA:
Cardiovascular Devices: Pacemakers and implantable defibrillators, Heart valves and vascular grafts, Left ventricular assist devices (LVADs), Coronary stents (some types)
Neurological Devices: Deep brain stimulators, Spinal cord stimulators, Implantable neurostimulators, Some epilepsy treatment devices
Orthopedic Implants: Hip and knee replacement systems, Spinal fusion hardware, Bone growth stimulators, Some trauma fixation devices
Ophthalmology Devices: Intraocular lenses, Retinal implants, Corneal transplant devices
Life-Support Equipment: Certain ventilators, Heart-lung bypass machines, Some dialysis equipment

Devices That Usually Don't Require PMA:
Class I and Most Class II Devices: Surgical instruments, Diagnostic equipment, Most medical software, External monitoring devices
510(k)-Exempt Devices: Simple medical devices with established safety profiles, Devices substantially equivalent to pre-1976 devices
How to Determine If Your Device Needs PMA
Check FDA's Product Classification Database to determine your device's regulatory pathway:
Search by device name or product code
Review the classification and regulation number
Check if PMA is required in the device description
Look for guidance documents specific to your device type
If your device is novel or doesn't fit existing classifications, FDA may require a De Novo petition to establish appropriate regulatory controls.
The PMA Process: Step by Step

Phase 1: Pre-Clinical Development (1-3 years)
Before human testing, develop comprehensive pre-clinical evidence:
Device Design and Development:
Finalize device design and manufacturing processes
Establish design controls and quality systems
Conduct comprehensive bench testing and validation
Perform biocompatibility testing for patient-contacting materials
Animal Testing (If Required):
Design animal studies to evaluate safety and performance
Conduct Good Laboratory Practice (GLP) studies
Generate data supporting transition to human studies
Address any safety concerns before clinical trials
Manufacturing Validation:
Establish manufacturing processes and controls
Validate sterilization and packaging methods
Demonstrate manufacturing consistency and quality
Prepare for commercial-scale production
Phase 2: Clinical Trial Planning (6-12 months)
Clinical trials are almost always required for PMA devices:
Investigational Device Exemption (IDE):
Submit IDE application to FDA before starting clinical trials
Describe study protocol, device design, and safety measures
Obtain Institutional Review Board (IRB) approval
Train clinical investigators and monitor study conduct
Clinical Trial Design:
Design studies to demonstrate safety and effectiveness
Determine appropriate endpoints and success criteria
Calculate required sample sizes for statistical significance
Plan for multiple study phases if needed
Phase 3: Clinical Trials (1-5 years)
Conduct clinical studies to generate effectiveness data:
Pilot Studies:
Small studies (20-100 patients) to evaluate initial safety
Refine device design based on early clinical feedback
Establish preliminary effectiveness signals
Identify potential safety concerns
Pivotal Trials:
Large studies (100-1,000+ patients) demonstrating effectiveness
Randomized controlled trials comparing to standard of care
Long-term follow-up to assess device durability
Multi-center studies to demonstrate broad applicability
Post-Market Studies (May Be Required):
Continue monitoring device performance after approval
Assess long-term safety and effectiveness
Study device performance in broader patient populations
Phase 4: PMA Submission Preparation (6-12 months)
Compile comprehensive PMA application:
Clinical Data Analysis:
Analyze all clinical trial data for safety and effectiveness
Perform statistical analysis demonstrating device performance
Compare results to appropriate control groups
Address any safety signals or adverse events
Manufacturing Information:
Document complete manufacturing processes and controls
Provide facility information and quality system details
Include device labeling and instructions for use
Demonstrate manufacturing consistency and validation
Phase 5: FDA Review Process (6-18 months)
Submit PMA and undergo FDA scientific review:
Administrative Review (45 days):
FDA determines if submission is complete for substantive review
Missing information requests may delay review start
FDA assigns review team and establishes review timeline
Scientific Review (180+ days):
FDA conducts comprehensive review of clinical and technical data
Multiple FDA divisions may participate in review process
FDA may request additional information or studies
Advisory panel meeting may be required for novel devices
FDA Decision:
Approval with or without conditions
Approvable letter requiring specific changes
Not approvable letter identifying deficiencies
Denial (rare, usually after multiple revision attempts)
Types of PMA Applications
Original PMA
Used for completely new devices without FDA-approved predecessors:
Requirements:
Complete clinical trial data demonstrating safety and effectiveness
Comprehensive manufacturing and quality information
Detailed device description and intended use
Risk analysis and benefit-risk assessment
Review Timeline: 6-18 months after submission acceptance
Success Rate: Ultimate approval rates now exceed 90 %, but only ~30-40 % of PMAs clear on the first review cycle.
PMA Supplement
Used for changes to already-approved PMA devices:
Panel-Track Supplement:
Significant changes requiring clinical data
New indications or patient populations
Major design or manufacturing changes
Review timeline: 180+ days
180-Day Supplement:
Moderate changes with supporting data
Labeling changes with clinical impact
Manufacturing changes affecting safety or effectiveness
Review timeline: 180 days
Minor changes with minimal risk impact
Administrative labeling changes
Manufacturing changes not affecting device performance
Review timeline: Typical FDA decision in ~60 days; there is no statutory clock, but the process is designed for a single, interactive review meeting.
Allows submission of PMA sections over time rather than all at once:
Benefits:
Earlier FDA feedback on study design and data requirements
Reduced risk of major submission problems
Opportunity to address FDA concerns before final submission
Requirements:
Pre-submission meetings to establish modular approach
Structured submission timeline agreed upon with FDA
Complete final module must still meet full PMA requirements
PMA vs. Other FDA Pathways
Understanding how PMA compares to other FDA pathways helps you choose the right approach for your device. More here.
PMA Costs and Timeline Planning
Typical PMA Development Costs
FDA User Fees (2025):
Standard business: $540,783 for original PMA
Small business: $135,196 for original PMA
Development and Clinical Costs (Estimation):
Pre-clinical development: $1-5 million
Clinical trials: $5-50 million (depending on complexity)
Regulatory consulting: $500,000-$2 million
Manufacturing validation: $1-5 million
Total typical cost: $10-100 million+
Pre-Clinical Phase: 1-3 years (design, testing, animal studies)
Clinical Trials: 2-5 years (pilot studies, pivotal trials)
PMA Preparation: 6-12 months (data analysis, submission writing)
FDA Review: 6-18 months (review, potential revisions)
Total Timeline: 4-8+ years from concept to approval
Factors That Affect Cost and Timeline
Faster/Less Expensive:
Device modifications to existing approved devices
Well-established clinical endpoints and study designs
Experienced clinical and regulatory teams
Clear FDA guidance for device category
Slower/More Expensive:
First-in-class devices requiring novel clinical approaches
Complex multi-component systems
Rare conditions requiring specialized clinical expertise
International regulatory requirements adding complexity

Common PMA Challenges and Solutions
Insufficient Clinical Evidence
The most common reason for PMA delays or denials is inadequate clinical data.
Common Problems:
Underpowered studies that don't demonstrate effectiveness
Inappropriate control groups or study designs
Insufficient follow-up time to assess device durability
Missing safety data for important patient subgroups
Solutions:
Invest in Pre-Submission meetings to align with FDA on study design
Use appropriate statistical methods and sample size calculations
Plan for longer follow-up periods than initially anticipated
Consider advisory panel feedback when designing trials
Manufacturing and Quality Issues
FDA expects robust manufacturing controls for PMA devices.
Common Problems:
Inadequate manufacturing validation and process controls
Inconsistent device performance across manufacturing lots
Insufficient quality system documentation
Manufacturing changes during clinical trials without proper validation
Solutions:
Implement comprehensive quality systems early in development
Validate manufacturing processes before starting clinical trials
Maintain detailed documentation of all manufacturing changes
Consider FDA Quality System Inspection readiness throughout development
Inadequate Risk-Benefit Analysis
FDA requires clear demonstration that device benefits outweigh risks.
Common Problems:
Insufficient characterization of device risks
Inadequate comparison to existing treatment options
Missing analysis of risk mitigation strategies
Unclear benefit quantification for patient populations
Solutions:
Conduct thorough risk analysis using ISO 14971 principles
Clearly define and quantify patient benefits in clinical terms
Compare your device to all relevant treatment alternatives
Engage clinical experts who understand current treatment limitations
PMA Post-Market Requirements
Ongoing FDA Obligations
PMA approval comes with significant post-market responsibilities:
Submit comprehensive annual reports summarizing device performance
Include adverse event data, complaint trends, and corrective actions
Report manufacturing changes and quality system updates
Provide updates on post-market studies if required
Report device malfunctions that could cause death or serious injury
Manufacturers must submit an MDR within 30 days of becoming aware of a reportable event
A 5-day report is required only if remedial action is needed to prevent serious public-health risk.
Maintain complaint files and investigate all reported problems
Implement corrective and preventive actions as needed
Complete any post-market studies required as condition of approval
Submit periodic progress reports and final study results
Modify device labeling based on post-market findings if required
PMA Supplements for Changes
Most changes to PMA devices require FDA approval through PMA supplements:
Changes Requiring Supplements:
New indications for use or patient populations
Significant design or manufacturing changes
Labeling changes with clinical implications
Manufacturing site changes or major process modifications
Change Planning:
Plan for PMA supplement costs and timelines when making changes
Consider cumulative impact of multiple changes on approval timeline
Maintain change control documentation for all device modifications
The Fastest Path to Market
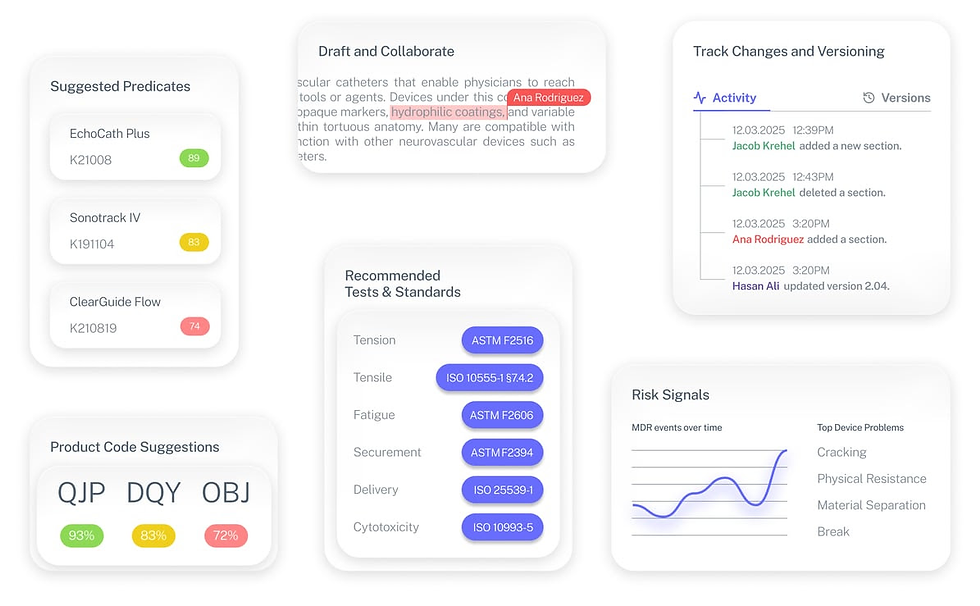
No more guesswork. Move from research to a defendable FDA strategy, faster. Backed by FDA sources. Teams report 12 hours saved weekly.
FDA Product Code Finder, find your code in minutes.
510(k) Predicate Intelligence, see likely predicates with 510(k) links.
Risk and Recalls, scan MAUDE and recall patterns.
FDA Tests and Standards, map required tests from your code.
Regulatory Strategy Workspace, pull it into a defendable plan.
👉 Start free at complizen.ai
Frequently Asked Questions
Q: Can I start selling my PMA device while under FDA review?
A: No. PMA devices cannot be marketed until FDA grants approval. Limited distribution is possible under Investigational Device Exemption (IDE) for clinical trials only.
Q: What happens if FDA denies my PMA?
A: FDA denial is possible. You can request a meeting to discuss FDA's concerns, address deficiencies, and potentially resubmit. Some companies pivot to different indications or patient populations based on FDA feedback.
Q: How do I know if my device needs clinical trials?
A: Nearly all PMA devices require clinical trials. The scope depends on device risk and available predicate data. Pre-Submission meetings with FDA help clarify clinical requirements early.
Q: Can foreign clinical data support a US PMA?
A: Yes, FDA accepts foreign clinical data if studies meet FDA's Good Clinical Practice standards and are relevant to the US patient population. Many companies conduct international trials to reduce costs and timelines.
Q: What's the difference between PMA approval and clearance?
A: PMA devices receive "approval" based on safety and effectiveness evidence. 510(k) devices receive "clearance" based on substantial equivalence. Approval requires more rigorous evidence than clearance.
Key Takeaways
PMA is FDA's most rigorous device pathway reserved for the highest-risk medical devices. It requires comprehensive clinical evidence proving safety and effectiveness.
Clinical trials are almost always required for PMA devices. Plan for 2-5 years of clinical development and $5-50 million in clinical costs.
Timeline planning is critical with total development taking 4-8+ years from concept to approval. Adequate funding for the entire journey is essential.
FDA user fees are substantial at $540,783 for standard businesses and $135,196 for small businesses, plus much higher development costs than other pathways.
Post-market obligations are extensive including annual reports, adverse event reporting, and potential post-market studies.
Early FDA engagement is crucial through Pre-Submission meetings to align on clinical requirements and avoid costly development mistakes.
Next Steps
Considering PMA for your device? Start with device classification confirmation and early FDA engagement to understand requirements.
Need PMA development strategy? Complizen's regulatory experts have guided numerous successful PMA approvals and can help you navigate this complex pathway efficiently.
Schedule a PMA strategy consultation or access our PMA development toolkit to plan your approval strategy.
Successful PMA approval requires early planning, adequate resources, and expert guidance. Our team helps you develop winning PMA strategies from concept through approval.


