How Much Does It Cost to Bring a Medical Device to Market? 2025 Budget Guide
- Beng Ee Lim

- Aug 3, 2025
- 8 min read
Updated: Oct 17, 2025
Medical device development costs vary by classification: Class I ($200K-$2M), Class II ($2M-$30M), and Class III ($5M-$119M+). Major expenses include clinical trials (40-60% of budget), regulatory activities (10-15%), manufacturing setup (15-25%), and commercialization (10-20%). Timeline spans 1-7 years depending on complexity and pathway.
The #1 question every medtech entrepreneur asks: "How much funding do I actually need?" The answer depends on your device classification, regulatory pathway, and clinical requirements.
Most startups dramatically underestimate total costs, leading to funding shortfalls that kill promising innovations. This guide provides realistic cost estimates based on industry data to help you plan properly.

Note: All cost figures in this guide are estimates based on industry studies and may vary significantly based on device complexity, regulatory pathway, and company-specific factors.
What Drives Medical Device Development Costs?
The brutal reality: medical device development is expensive because failure costs lives. Unlike software that can be patched post-launch, medical devices must work perfectly from day one.
Device Classification Determines Everything
Your FDA device classification drives every cost decision:
Class I (Low Risk)
Estimated Total Cost: $200K-$2M
Estimated Timeline: 12-24 months
Regulatory Path: 510(k) exempt or simple 510(k)
Examples: Bandages, tongue depressors, examination gloves
Class II (Moderate Risk)
Estimated Total Cost: $2M-$30M
Estimated Timeline: 24-48 months
Regulatory Path: 510(k) clearance, some require clinical data
Examples: Infusion pumps, surgical drapes, pregnancy test kits
Class III (High Risk)
Estimated Total Cost: $5M-$119M+
Estimated Timeline: 36-84 months
Regulatory Path: PMA with extensive clinical trials
Examples: Heart valves, pacemakers, breast implants
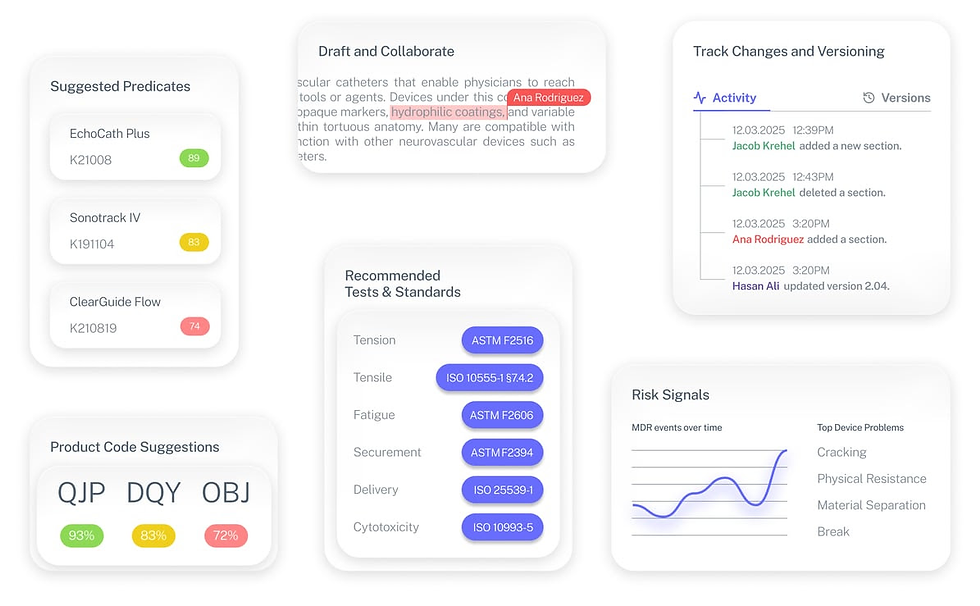
💡 A modern way to approach cost planning
Many of these early expenses stem from time-consuming research - identifying the right classification, product code, and potential predicate devices.
Tools like Complizen streamline this process by automatically mapping product codes, related predicates, and testing requirements, helping teams plan more accurately and allocate budgets with confidence.
The Real Cost Drivers
Clinical Trials (Estimated 40-60% of Total Budget)
Complex medical devices require clinical studies costing an estimated $32.1 million on average, representing 59% of R&D expenditures according to ASPE research. Simple devices may need no clinical data, while high-risk devices require multi-year pivotal studies.
Regulatory Pathway Complexity
FDA user fees increased 11.8% from 2024 to 2025, with registration fees jumping 21.3% to $9,280. PMA submissions now cost $445,000 in user fees alone according to the Federal Register.
Technology Innovation Level
Me-too devices leverage existing predicate data. Breakthrough technologies require extensive validation, safety testing, and novel clinical endpoints.
FDA User Fees Breakdown 2025
Here's exactly what you'll pay the FDA for regulatory review:
Current Fee Schedule (FY 2025)
Submission Type | Standard Fee | Small Business Fee |
510(k) Submission | $24,335 | $6,084 |
De Novo Request | $162,235 | $40,559 |
PMA, PDP, PMR, BLA | $540,783 | $135,196 |
Annual Registration | $9,280 | No reduction available |
Small Business Qualifications
Based on FDA Small Business Determination (SBD) Program guidelines
Reduced Fees: Companies with ≤$100 million annual revenue qualify for 75% fee reduction Fee Waivers: Companies with ≤$30 million annual revenue can waive their first PMA fee
No Shortcuts: Small business certification must be obtained through FDA's Small Business Determination (SBD) program before submission
Hidden Fee Realities
Multiple Submissions: Complex devices often require 2-3 submissions before approval
Supplement Fees: Post-market changes trigger additional fees
International Fees: CE marking, Health Canada, and other markets add separate costs
Phase-by-Phase Cost Breakdown
Concept & Design (Estimated 8-15% of Total Budget)
What Happens: Market research, concept validation, initial design
Estimated Timeline: 12-20 months
Typical Cost Estimates: $300K-$5M
Key Expenses:
Market research and competitive analysis
Intellectual property searches and filing
Initial prototype development
Design controls documentation
FDA Q-submission consultations
A large portion of early costs come from manual research — finding classification, product codes, and potential predicates. Complizen’s Product Code Finder and Predicate Intelligence automate this early groundwork, saving weeks of consultant time before testing even begins.
Development & Testing (Estimated 20-30% of Total Budget)
What Happens: Product development, verification, validation testing
Estimated Timeline: 12-24 months
Typical Cost Estimates: $1M-$10M
Major Cost Components:
Engineering design and development
Biocompatibility testing (ISO 10993)
Electrical safety testing (IEC 60601)
Software validation (IEC 62304)
Sterilization validation
Packaging validation
Identifying which tests and standards apply is often where founders overspend. Complizen’s Tests & Standards module cross-references FDA-recognized standards used by similar cleared devices, so you can design your test plan confidently and avoid redundant testing.
Clinical Trials (Estimated 40-60% of Total Budget)
What Happens: Human testing to demonstrate safety and effectiveness
Estimated Timeline: 12-36 months
Typical Cost Estimates: $2M-$50M+
Cost Drivers by Study Type:
Feasibility Studies
Patient Count: 10-50 patients
Estimated Cost Range: $500K-$2M
Purpose: Proof of concept, dose finding
Pivotal Studies
Patient Count: 100-1,000+ patients
Estimated Cost Range: $5M-$50M+
Purpose: Definitive safety and effectiveness data
Clinical trial site costs range from $3,500-$7,500 in startup fees, plus an average of $41,413 per patient according to ISMP research. Each patient visit costs an estimated median of $3,685.
Regulatory Submission (Estimated 2-8% of Total Budget)
What Happens: Preparing and submitting FDA application
Estimated Timeline: 6-12 months
Typical Cost Estimates: $500K-$3M
What You're Really Paying For:
Regulatory consulting and strategy
Technical writing and documentation
FDA user fees
Response to FDA questions
Advisory panel preparation (if required)
Manufacturing Scale-Up (Estimated 15-25% of Total Budget)
What Happens: Transitioning from prototype to commercial production
Estimated Timeline: 12-18 months
Typical Cost Estimates: $2M-$20M
Hidden Manufacturing Realities:
Quality system implementation (ISO 13485)
Manufacturing validation and process controls
Supply chain qualification
Initial inventory investment
Post-market surveillance systems

Hidden Costs That Destroy Budgets
The 50% Rule: Plan for Cost Overruns
Budget Reality Check: When accounting for capital costs and failure rates, complex device development costs can reach $526.4 million according to ASPE research. Smart companies budget 150% of initial estimates.
Post-Market Surveillance (Often Forgotten)
Estimated Annual Costs: $100K-$1M+ per year
Requirements: Adverse event reporting, periodic safety updates, complaint handling Reality: These costs continue for the product's entire lifecycle
International Market Access
Europe (CE Marking): Estimated $220 K–660 K additional
Canada (Health Canada): Estimated US $20-60 K additional
Asia-Pacific Markets: Estimated $100K-$300K per major market
Quality System Maintenance
ISO 13485 Certification: Estimated US $30-75 K up front and US $5-10 K yearly for audits
Design Controls: Expect 10-15 % of total dev. budget
Risk Management (ISO 14971): Estimated US $20-50 K
Cost Comparison by Device Type
Software as Medical Device (SaMD)
Class I-II Software
Estimated Development: $500K-$3M
Clinical: Often none required
Regulatory: $13,108-$122,380 in fees
Estimated Total: $1M-$5M
Class III Software
Estimated Development: $2M-$10M
Clinical: $5M-$30M
Regulatory: $500,000+ in fees
Estimated Total: $10M-$50M+
Implantable Devices
Simple Implants (Orthopedic)
Estimated Development: $3M-$8M
Clinical: $10M-$30M
Manufacturing: $5M-$15M
Estimated Total: $20M-$60M
Active Implants (Pacemakers)
Estimated Development: $10M-$30M
Clinical: $30M-$100M
Manufacturing: $10M-$30M
Estimated Total: $60M-$200M+
Diagnostic Devices
Point-of-Care Tests
Estimated Development: $1M-$5M
Clinical: $2M-$10M
Manufacturing: $2M-$8M
Estimated Total: $5M-$25M
Laboratory Instruments
Estimated Development: $5M-$20M
Clinical: $10M-$40M
Manufacturing: $5M-$20M
Estimated Total: $25M-$100M
How to Reduce Development Costs
Strategic Planning Framework
Start with End in Mind
Define target product profile early
Identify regulatory pathway before development
Plan clinical strategy during design phase
Budget for 150% of initial estimates
Most of these expenses — testing, consultant hours, and documentation — stem from information gathering and uncertainty early on. Automating the discovery phase with Complizen helps startups make earlier, data-backed decisions that directly lower total submission costs.
Leverage FDA Programs
Breakthrough Device Designation
Benefit: Accelerated review, enhanced communication
Cost Impact: Can reduce timeline by 6-12 months
Savings: $2M-$10M in reduced development costs
Q-Submission Program
Benefit: FDA guidance reduces late-stage surprises
Estimated ROI: Average prep outlay (consultant + staff) runs US $10-40 k, yet avoids six-figure rework by clarifying test plans early.
Adaptive Trial Design
Simplified clinical protocols could reduce costs by an estimated 33.4% according to ASPE research. Use interim analyses to modify studies and implement seamless Phase II/III designs.
Registry Studies
Leverage existing patient databases
Reduce patient recruitment costs
Accelerate enrollment timelines
International Harmonization
Single Global Study Design
Meet FDA, CE marking, and other requirements simultaneously
Use ICH guidelines for standardization
Coordinate with multiple regulatory bodies early
Funding Strategy by Development Stage
Pre-Seed Funding ($0.2-2 M)
What It Covers: fuels concept validation, provisional patents, breadboard prototypes.
Investor Focus: Proof of concept, market need validation
Milestone: Working prototype, initial IP protection
Seed Funding ($2M-$7M)
What It Covers: backs design-freeze, benchtop V&V, pre-clinical GLP studies, 510(k)/De Novo
Investor Focus: Technical feasibility, regulatory pathway clarity
Milestone: Design freeze, preclinical data package
Series A ($10M-$30M)
What It Covers: funds first-in-human (IDE) trials, Q-sub meetings, pilot manufacturing line
Investor Focus: Clinical data, regulatory approval pathway
Milestone: First-in-human data, FDA submission acceptance
Series B ($30M-$50M+)
What It Covers: bankrolls pivotal trials, commercial-grade tooling, inventory build, market access prep
Investor Focus: Pivotal trial results, commercial viability
Milestone: Regulatory approval, commercial launch readiness
ROI Timeline and Revenue Expectations
Break-Even Analysis
Class I Devices: 2-3 years post-launch
Class II Devices: 3-5 years post-launch
Class III Devices: 5-8 years post-launch
Revenue Ramp Expectations
Year 1: 10-20% of peak sales potential
Year 2: 30-50% of peak sales potential
Year 3: 60-80% of peak sales potential
Year 4+: Peak sales achievement
Market Size Requirements
Minimum Market: $100M+ total addressable market for VC interest
Success Threshold: $50M+ annual revenue at peak for meaningful exit
Competition Factor: First-mover advantage worth 2-3x revenue multiple
What This Means for Your Medical Device Company
Budget Planning Reality Check
Don't Underestimate: Total company funding for Class II devices averages an estimated $30 million, with development costs of $2-5 million representing just a fraction of total investment
Plan for Failures: Most submissions pass, but company attrition is brutal—only ~1 in 4 start-ups ever files. Build runway for pivots & kill-points, not just regulatory risk.
Timeline Expectations: Add 50% buffer to all timeline estimates
Critical Success Factors
Early Regulatory Engagement
Schedule FDA pre-submission meetings
Understand requirements before significant investment
Plan international strategy from day one
Clinical Strategy Optimization
Design studies to meet multiple regulatory requirements
Use adaptive designs to minimize risk
Leverage real-world evidence where possible
Quality System Investment
Implement design controls early
Build quality into development process
Plan for post-market requirements
Ready to Navigate Medical Device Development Costs?
Understanding development costs is just the beginning. The path from concept to market requires strategic planning, regulatory expertise, and careful resource management.
Smart medical device companies partner with regulatory experts early to avoid the expensive mistakes that kill promising innovations.
The Fastest Path to Market
Complizen helps startups and consultants build their regulatory strategy in minutes, backed by FDA sources — cutting weeks of prep and thousands in consultant costs.
No more guesswork. Move from research to a defendable FDA strategy, faster.
FDA Product Code Finder, find your code in minutes.
510(k) Predicate Intelligence, see likely predicates with 510(k) links.
Risk and Recalls, scan MAUDE and recall patterns.
FDA Tests and Standards, map required tests from your code.
Regulatory Strategy Workspace, pull it into a defendable plan.
👉 Start free at complizen.ai
Frequently Asked Questions
What's the cheapest way to get FDA clearance?
510(k) clearance for Class II devices with substantial equivalence to existing products. Estimated costs range from $500K-$2M total if no clinical data required.
How much should we budget for regulatory consulting?
Industry estimates suggest 15-25% of total development budget for regulatory expertise. Don't skimp—poor regulatory strategy costs far more than expert guidance.
What costs can be reduced without compromising quality?
Leverage existing clinical data, use adaptive trial designs, coordinate international requirements, and implement quality systems early to avoid rework.
When do we need to pay FDA user fees?
Fees must be paid before FDA begins review. Budget for payment 30-60 days before submission to avoid delays.
How long does regulatory approval actually take?
FDA target timelines: 510(k): 90 days, De Novo: 150 days, PMA: 180 days after submission. Add 6-12 months for submission preparation.


