Clinical Evidence for SaMD: Valid Association, Analytical & Clinical Validation
- Beng Ee Lim

- Jun 10, 2025
- 3 min read
Updated: Sep 7, 2025
To structure SaMD clinical evidence, build three pillars: valid clinical association (link SaMD output to the condition), analytical validation (technical accuracy/robustness), and clinical validation (benefit/performance in the target population). The rigor scales with your SaMD risk category (significance of information × condition seriousness). Define clear endpoints, populations, and stats up front.

Why Clinical Evidence Matters for SaMD
FDA’s latest guidance signals a shift: for SaMD that influences clinical decisions, real-world performance data is becoming non-negotiable.
Incomplete or misaligned evidence is the #1 driver of Additional Information (AI) requests.
The 2025 draft prioritizes fit-for-purpose evidence tied to device function, patient impact, and risk class.
A well-structured clinical evidence plan is your submission's foundation—and credibility booster.
Tiers of Clinical Evidence
Tier | Purpose | Study Type | Key Deliverables |
Analytical Validation | Confirm algorithm performance on known data | Bench testing; retrospective simulation | Accuracy metrics; confusion matrix |
Retrospective Clinical Review | Assess performance on historical data | Chart review; registry analysis | Sensitivity/specificity tables; study summary |
Prospective Observational Study | Demonstrate real-world use | Single-arm observational cohort | Clinical study report; endpoint analysis |
Controlled Prospective Trial | Compare against standard of care | Randomized or matched cohort trial | Controlled trial report; statistical analysis |
Designing Your Clinical Evidence Plan
Step 1: Define Intended Use and Target Population
Clearly specify the SaMD’s clinical purpose (e.g., diagnosis, triage, monitoring, prediction).
Define the clinical setting (e.g., ICU, outpatient, primary care).
Detail inclusion and exclusion criteria for the intended users and patient population.
This step ensures the evidence generated is relevant to the real-world use case.
Step 2: Establish Valid Clinical Association
Demonstrate that the SaMD output is scientifically and clinically associated with the targeted clinical condition or physiological state.
Use existing literature, clinical guidelines, or generate new evidence if novel.
This forms the foundation for all further validation steps.
Step 3: Select Study Endpoints and Metrics
Choose primary endpoints that reflect clinical relevance, such as diagnostic accuracy (sensitivity, specificity), time-to-alert, or prediction performance.
Include secondary endpoints like impact on provider workflow, usability, or time saved.
Define measurable, clinically meaningful metrics aligned with intended use.
Step 4: Plan Analytical Validation
Design tests to verify the SaMD processes input data correctly and produces accurate, reliable, and precise outputs.
Use bench testing, simulations, or retrospective data.
Document accuracy metrics, confusion matrices, and error rates.
Step 5: Plan Clinical Validation
Design studies to demonstrate clinical performance and impact in the target population and setting.
Possible study designs include retrospective clinical reviews, prospective observational studies, or controlled trials.
Collect data on clinical outcomes, usability, and safety.
Step 6: Define Statistical Methods and Sample Size
Calculate sample sizes with adequate statistical power to detect meaningful effects.
Plan confidence intervals and subgroup analyses (e.g., by age, sex, comorbidities).
Ensure statistical rigor to support regulatory submissions and clinical claims.
Step 7: Identify Data Sources and Quality Control Measures
Determine data sources such as electronic health records (EHRs), device logs, clinical registries, or structured case report forms (CRFs).
Implement SOPs for data extraction, curation, and quality assurance.
Use validated data collection tools with audit trails to ensure data integrity.
Step 8: Execute Evidence Generation and Documentation
Conduct analytical and clinical validation activities per plan.
Analyze data using appropriate statistical methods.
Document results thoroughly in clinical evaluation reports following regulatory standards.
Step 9: Engage with Regulatory Authorities and Plan Lifecycle Management
Seek early and ongoing feedback from regulators to ensure alignment.
Plan for continuous clinical evaluation, including post-market surveillance and real-world data collection.
Update clinical evidence as the SaMD evolves or new clinical insights emerge.
The Fastest Path to Market
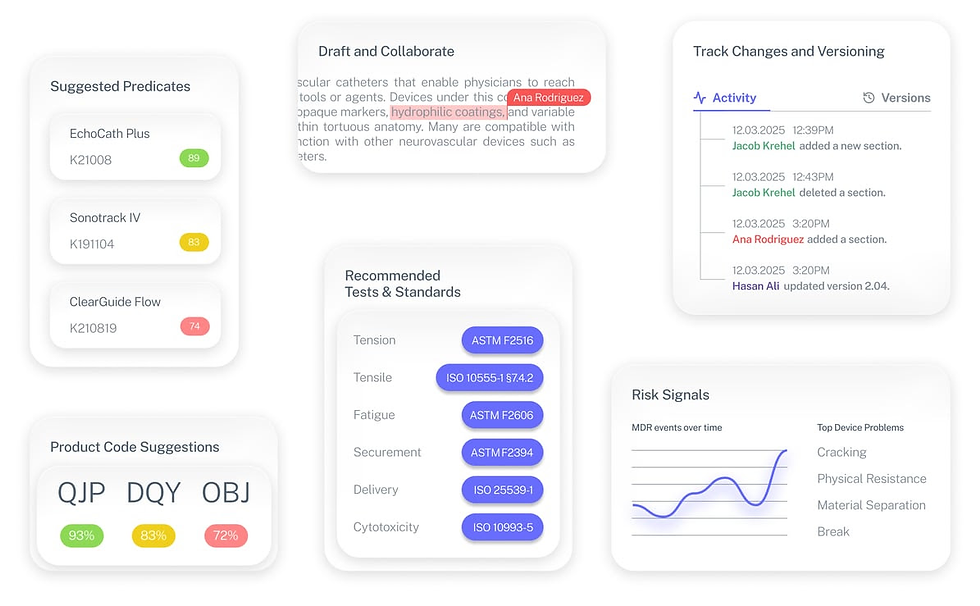
No more guesswork. Move from research to a defendable FDA strategy, faster. Backed by FDA sources. Teams report 12 hours saved weekly.
FDA Product Code Finder, find your code in minutes.
510(k) Predicate Intelligence, see likely predicates with 510(k) links.
Risk and Recalls, scan MAUDE and recall patterns.
FDA Tests and Standards, map required tests from your code.
Regulatory Strategy Workspace, pull it into a defendable plan.
👉 Start free at complizen.ai
FAQ
What level of evidence is enough for a 510(k)?
For moderate-risk SaMD (IMDRF Cat II–III), retrospective + prospective observational evidence with analytical validation is typically sufficient.
Do I always need a controlled trial?
No. Controlled trials are ideal for high-risk SaMD (Cat IV) but not always required if strong real-world data exists.
Can real-world evidence replace prospective studies?
Not entirely. Real-world data can supplement but not replace planned studies unless justified via Pre-Sub.


