What Is IMDRF? 2025 AI/ML & SaMD Guide (N88 GMLP + N81 Risk)
- Aug 11, 2025
- 6 min read
Updated: Sep 7, 2025
IMDRF is the global forum harmonizing medical device regulations across major markets (FDA, MHRA, Health Canada, EU). On Jan, 2025, IMDRF finalized N88 (10 Good Machine Learning Practice principles for AI/ML devices) and N81 (characterization considerations for medical-device software and software-specific risk). IMDRF documents guide—but don’t replace—jurisdictional rules; adoption timing varies by regulator.
This guide covers everything you need to know about IMDRF's impact on AI medical devices, SaMD regulation, and how to implement their frameworks before your competition.

What Is IMDRF and Why Should You Care?
The International Medical Device Regulators Forum brings together the world's major medical device regulators to harmonize requirements globally. IMDRF Management Committee regulators include Australia, Brazil, Canada, China, the EU, Japan, Russia, Singapore, South Korea, Switzerland, the UK, and the US FDA.
Here's why IMDRF matters for your business: IMDRF documents are non-binding but highly influential. Regulators often reference or align with them over time — this means IMDRF guidance gives you a preview of future regulatory requirements across multiple markets.
IMDRF's January 2025 AI Breakthrough
In January 2025, IMDRF released two critical documents that will reshape AI medical device regulation:
IMDRF/AIML WG/N88 FINAL:2025 - Good Machine Learning Practice (GMLP) principles
IMDRF/SaMD WG/N81 FINAL:2025 - Characterization Considerations for Medical Device Software and Software-Specific Risk
The bottom line: These aren't just guidance documents. They're the roadmap that global regulators will use to evaluate AI medical devices. Companies implementing these frameworks now will have significant competitive advantages.
What Are IMDRF's 10 Good Machine Learning Practice Principles?
IMDRF N88 (2025) sets out 10 GMLP principles that AI medical device manufacturers must follow. These principles are already aligned with FDA, MHRA, and Health Canada, meaning implementation prepares you for multiple regulatory submissions.
The 10 GMLP Principles:
1. Multidisciplinary expertise across the TPLC.
Keep clinical, data science, engineering, RA/QA, and human-factors experts engaged from concept through post-market.
2. Good Software Engineering and Security Practices
Run a secure SDLC (config/version control, code review, threat modeling, reproducible builds, secure release).
3. Use Representative Participants & Datasets
Make data and study populations match the intended patients, setting, devices, and real-world variability.
4. Ensure Train/Test Independence
Prevent data leakage with strict separation of training/validation/test sets; lock test sets before tuning.
5. Use Fit-for-purpose Reference Datasets
Use benchmarks/ground truth with clear provenance, best-available methods, strong labeling quality, and versioning.
6. Model Design Reflects Intended Use & Available Data.
Align architecture/features with indications, inputs, workflow, and data quality/volume.
7. Focus Is Placed on the Performance of the Human-AI Team
Design UI, alerts, and mitigations that improve clinician+AI outcomes; validate teamwork, not just the model.
8. Clinically Relevant Testing
Demonstrate performance under realistic conditions (multi-site/device, protocol variability, noise, expected distribution shift).
9. Users Are Provided Clear, Essential Information
Provide intended use/users, inputs & acceptable ranges, performance (including subgroups), limitations, and warnings.
10. Post-deployment Monitoring & Retaining Risk Mangement
Track drift/bias/failure modes, define update triggers, and manage changes under QMS (e.g., via PCCP where applicable).
How Does IMDRF's Software Risk Framework Work?
The N81 document provides the most comprehensive software risk characterization framework ever published by IMDRF. This framework expands beyond traditional SaMD to include all medical device software, including embedded software.
Key Risk Characterization Categories:
Medical Problem and Objective
Medical purpose (diagnosis, treatment, monitoring, prevention)
Intended disease or condition severity
Target patient population characteristics
Context of Use
Intended user type and expertise level
Use environment (clinical vs. home use)
Timing within healthcare workflow
Role in clinical decision-making
Software Function and Use
Output type (clinical interpretation, workflow recommendation, data processing)
Input sources and data dependencies
Degree of autonomy (autonomous, supervised, non-autonomous)
Explainability and transparency level
Change Management
Learning and update mechanisms
Domain-specific implementation requirements
Distribution and installation infrastructure
Critical Risk Assessment Questions
The framework includes specific questions manufacturers must address:
Clinical Impact: Could software output lead to death, irreversible harm, or serious deterioration?
Workflow Integration: Does the software create single points of failure in clinical processes?
User Dependency: Can intended users understand and appropriately act on software outputs?
Data Quality: Are input sources reliable and representative of intended use populations?
What This Means for Different Medical Device Types
AI-Powered Diagnostic Software
High-Risk Considerations:
Autonomous diagnostic decisions without clinical oversight
Use in critical or emergency care settings
Complex algorithms with limited explainability
Implementation Strategy:
Focus on transparency and clinical validation
Implement robust performance monitoring
Design for appropriate clinical oversight
Software as a Medical Device (SaMD)
Key Requirements:
Comprehensive intended use statements
Clear output type classification
Appropriate user training and support
Regulatory Pathway Impact:
Better-characterized software may qualify for streamlined review
Poor characterization leads to additional regulatory questions and delays
AI-Enhanced Medical Devices
Integration Challenges:
Software risk must be evaluated within overall device risk
Consider interactions between AI components and hardware
Address cybersecurity and data privacy requirements
How to Implement IMDRF Frameworks in Your Organization
Phase 1: Assessment (Month 1)
Evaluate Current State:
Review existing products against GMLP principles
Identify gaps in documentation and processes
Assess team expertise and training needs
Key Deliverables:
Gap analysis report
Implementation roadmap
Resource allocation plan
Phase 2: Foundation Building (Months 2-4)
Establish Core Capabilities:
Implement data management frameworks
Develop risk characterization templates
Create multidisciplinary team structures
Critical Success Factors:
Executive leadership commitment
Cross-functional collaboration
Adequate resource allocation
Phase 3: Integration and Validation (Months 5-8)
Integrate into Development Processes:
Update design controls and procedures
Implement continuous monitoring systems
Validate framework effectiveness
Measurement and Monitoring:
Track regulatory submission outcomes
Monitor post-market performance
Measure development efficiency improvements
Regional Implementation Differences
United States (FDA)
Current Status: FDA guidance closely aligns with IMDRF GMLP principles
Implementation Timeline: No fixed adoption date.
Key Considerations: Focus on predetermined change control plans for AI/ML updates
United Kingdom (MHRA)
Current Status: MHRA is moving to IMDRF-aligned SaMD risk categorization as part of its regulatory refresh
Unique Advantage: Some low-risk Class I AI/ML devices may qualify for self-certification
Implementation Timeline: Phased implementation underway
European Union
Additional Requirements: EU AI Act compliance for high-risk medical AI applications
Timeline: Coordinate IMDRF implementation with AI Act requirements
Key Difference: More stringent transparency and explainability requirements
Canada (Health Canada)
Alignment Level: High alignment with IMDRF principles
Focus Areas: Emphasis on clinical validation and post-market surveillance
Implementation: Final MLMD guidance is in effect; integrate with standard device licensing pathways.
Common Implementation Mistakes to Avoid
Technical Implementation Errors
Inadequate Data Documentation
Failing to document training data sources and characteristics
Insufficient data version control
Poor handling of bias and representativeness issues
Weak Risk Characterization
Generic risk assessments that don't address software-specific hazards
Insufficient consideration of clinical workflow integration
Overlooking indirect harms and failure modes
Organizational Mistakes
Siloed Implementation
Treating IMDRF compliance as purely regulatory requirement
Failing to integrate with product development processes
Inadequate cross-functional team involvement
Resource Underestimation
Insufficient budget allocation for implementation
Unrealistic timeline expectations
Inadequate training and capability building
Future Outlook and Recommendations
Regulatory Trends
Global Harmonization Acceleration
Expect broader adoption of IMDRF frameworks across emerging markets
Increasing alignment between regional requirements
Enhanced focus on post-market surveillance and real-world performance
AI-Specific Developments
More detailed guidance on specific AI/ML applications
Enhanced requirements for bias detection and mitigation
Stronger emphasis on clinical validation and utility
Strategic Recommendations
For Startups:
Implement IMDRF frameworks from product conception
Build regulatory strategy around global harmonization
For Established Companies:
Conduct comprehensive gap analysis of existing products
Prioritize implementation for products entering new markets
Consider framework adoption for competitive advantage
For Regulatory Professionals:
Develop expertise in IMDRF frameworks before peers
Build relationships with global regulatory consultants
Stay current with implementation guidance from member regulators
The Fastest Path to Market
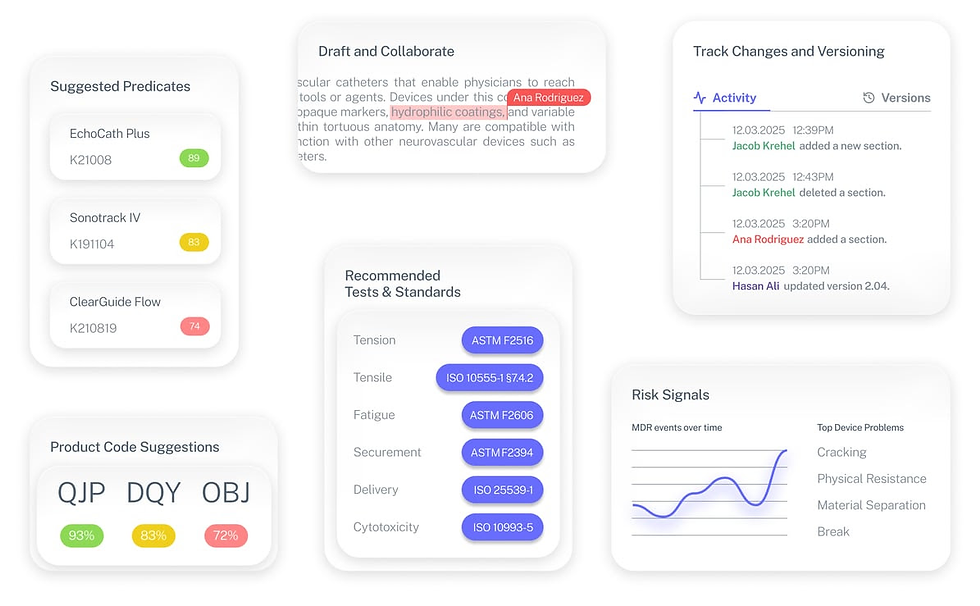
No more guesswork. Move from research to a defendable FDA strategy, faster. Backed by FDA sources. Teams report 12 hours saved weekly.
FDA Product Code Finder, find your code in minutes.
510(k) Predicate Intelligence, see likely predicates with 510(k) links.
Risk and Recalls, scan MAUDE and recall patterns.
FDA Tests and Standards, map required tests from your code.
Regulatory Strategy Workspace, pull it into a defendable plan.
👉 Start free at complizen.ai
Frequently Asked Questions
When will IMDRF guidance become mandatory?
IMDRF guidance isn't directly mandatory, but member regulators typically adopt similar requirements within 1-2 years. Companies should implement frameworks now to prepare for future requirements.
Do IMDRF frameworks apply to all software medical devices?
The N81 framework applies to all medical device software, including SaMD and embedded software. The N88 AI guidance applies specifically to ML-enabled medical devices.
How does IMDRF guidance differ from existing FDA requirements?
IMDRF guidance is closely aligned with current FDA requirements but provides more detailed implementation guidance and international perspective.
Can small companies realistically implement these frameworks?
Yes, but implementation should be scaled appropriately. Focus on core principles most relevant to your products and build capabilities gradually.
What's the biggest mistake companies make with IMDRF implementation?
Treating it as a checkbox compliance exercise rather than integrating frameworks into product development processes from the beginning.


