Do I Need FDA Approval, Clearance, or Exemption? 2025 Medical Device Guide
- Beng Ee Lim

- Aug 14, 2025
- 6 min read
Updated: Oct 17, 2025
Whether you need FDA approval, FDA clearance, or no regulatory submission at all depends on your device's risk classification and intended use. FDA approval (PMA) is required for high-risk Class III devices. FDA clearance (510(k)) is needed for most Class II devices and some Class I devices. However, most Class I devices and many Class II devices are exempt from premarket submissions but still require FDA registration and listing.
This guide provides a complete decision framework to determine exactly what FDA requirements apply to your medical device.

FDA Approval vs. Clearance vs. Exemption: Understanding the Difference
The biggest misconception in medical device regulation is thinking all devices need "FDA approval." In reality, the FDA uses three distinct regulatory pathways with very different requirements and timelines.
FDA Approval (PMA - Premarket Approval)
What it is: Full scientific review demonstrating safety and effectiveness through clinical trials and comprehensive data.
Required for: High-risk Class III medical devices without substantial equivalence to existing devices.
Timeline: 12-18 months average
Examples: Heart valves, implantable defibrillators, breast implants
FDA Clearance (510(k) - Premarket Notification)
What it is: Demonstration that your device is "substantially equivalent" to a legally marketed predicate device.
Required for: Most Class II devices and some Class I devices deemed higher risk.
Timeline: 3-6 months average
Examples: MRI machines, pulse oximeters, blood glucose monitors
No Premarket Submission Required (Exempt Devices)
What it is: Devices that can be marketed immediately after FDA registration and listing.
Applies to: Most Class I devices and select Class II devices exempted under FDAMA or Cures Act.
Timeline: 1-2 weeks for registration
Cost: $11,423 (Annual Establishment Registration Fee)
Examples: Bandages, examination gloves, stethoscopes, some software applications
The FDA Decision Tree: 4 Steps to Determine Your Requirements
Step 1: Is Your Product a Medical Device?
FDA Definition: An instrument, apparatus, implement, machine, contrivance, implant, in vitro reagent, or other similar article intended for use in the diagnosis, cure, mitigation, treatment, or prevention of disease.
Key Questions:
Does it diagnose, treat, cure, mitigate, or prevent disease?
Is it intended for use in the structure or function of the body?
Does it achieve its primary intended purpose through chemical action or metabolism?
Important Exception: Medical Device Data Systems (MDDS) software functions are not devices; MDDS hardware is Class I, typically 510(k)-exempt.
If NOT a medical device: No FDA submission required (but may need other regulatory oversight)
If YES a medical device: Proceed to Step 2
Step 2: What is Your Device Classification?
The FDA classifies medical devices into three risk-based categories that determine regulatory requirements.
Class I - Low Risk (47% of all medical devices)
Minimal potential for harm
Simple design and well-understood technology
Examples: Bandages, elastic bandages, manual surgical instruments
Class II - Moderate Risk (43% of all medical devices)
Moderate potential for harm
Require special controls (standards, labeling, post-market surveillance)
Examples: X-ray machines, infusion pumps, surgical drapes
Class III - High Risk (10% of all medical devices)
High potential for harm or life-threatening risk
Most complex regulatory requirements
Examples: Heart valves, pacemakers, HIV self-test kits
How to Check: Use FDA's Product Classification Database
Step 3: Check Exemption Status
Even if your device falls into Class I or II, it may be exempt from premarket submission requirements.
Class I Exemptions: FDA has exempted almost all Class I devices from the premarket notification requirement. Exceptions include "reserved devices" that pose substantial risk despite low classification.
Class II Exemptions: The FDA has exempted many Class II devices from 510(k) requirements under the 1997 FDAMA and 2016 Cures Act. These devices are considered "low-medium risk" where FDA can redirect resources to more significant public health issues.
How to Check Exemption Status:
Review FDA's Medical Device Exemptions database
Check 21 CFR Parts 862-892 for your device category
Verify no partial limitations apply to your specific device
Step 4: Consider Special Circumstances
Preamendment Devices: Preamendment (“grandfathered”) devices with the same intended use generally don’t require 510(k). Class III preamendment device types may later require PMA once FDA issues a call for PMA; until then, new entrants typically use 510(k).
Substantial Equivalence: Class III devices substantially equivalent to preamendment Class III devices may qualify for 510(k) instead of PMA (rare but possible).
Significant Changes: For exempt devices, you must submit a 510(k) if your change exceeds the .9 limitations (e.g., new intended use or different fundamental technology).
Common Scenarios: Real Examples of FDA Requirements
Software and Digital Health
Medical Device Data Systems (MDDS): Most MDDS software functions are ‘non-device’ under FD&C 520(o) or low risk under FDA policy, while MDDS hardware remains a Class I, 510(k)-exempt device. Registration/listing and QSR may still apply depending on the function
Clinical Decision Support Software: If it meets the 4 Non-Device CDS criteria → no FDA device oversight; otherwise expect Class II with 510(k) (or De Novo) and special controls
AI Diagnostic Tools: Most launch as Class II (De Novo then 510(k) predicates); check FDA’s AI/ML device list for precedents in your indication
Mobile Health Apps: First decide if the function is a ‘device’ under 520(o). If device, classification depends on risk and intended use; many end up Class II with 510(k)
Surgical and Diagnostic Equipment
Manual Surgical Instruments: Usually Class I exempt
Powered Surgical Instruments: Typically Class II requiring 510(k)
Implantable Devices: Expect Class III PMA unless your exact device type has been down
Diagnostic Imaging: Core systems (CT, fluoro, ultrasound) are Class II with 510(k); only certain accessories are Class I & exempt
Consumer Health Products
Home Pregnancy Tests: Class II requiring 510(k)
Blood Pressure Monitors: Class II requiring 510(k)
Digital Thermometers: Class II; some models are now 510(k)-exempt under 2025 FDA order
Contact Lenses: Daily-wear soft lenses (Class II, often 510(k)); extended-wear & IOLs (Class III, PMA)
Laboratory and Diagnostic
Laboratory Reagents: Classification varies, many Class I exempt
Genetic Testing Systems: Frequently Class II (De Novo + special controls → subsequent 510(k)s), but classification varies by intended use (some PMA)
Point-of-Care Diagnostics: Usually Class II requiring 510(k)
Specimen Collection Devices: Often Class I exempt
What You Still Need Even If You're Exempt
Being exempt from FDA premarket submission doesn't mean you're exempt from all FDA requirements.
Mandatory Requirements for All Medical Devices
Establishment Registration and Device Listing:
Register manufacturing facility with FDA
List each device you manufacture
Update annually and notify of changes
Cost: $11,423
Quality System Regulation (QSR/cGMP):
Most devices must comply with 21 CFR 820
Some Class I devices with asterisk (*) are exempt from full QSR
Exceptions: Record keeping (820.180) and complaint files (820.198) always required
Labeling Requirements:
FDA labeling regulations under 21 CFR 801
Adequate directions for use
Warnings and contraindications where applicable
Adverse Event Reporting:
Medical Device Reporting (MDR) requirements
Report serious injuries and malfunctions
Maintain complaint files and investigation records
GMP and QSR Exemptions
Class I devices marked with asterisk (*) in FDA exemption lists are also exempt from full GMP requirements, except:
Record keeping requirements (21 CFR 820.180)
Complaint file requirements (21 CFR 820.198)
If device is labeled as sterile, full GMP applies
If device contains software, full GMP applies
Strategic Decision Framework
Evaluate Your Business Goals
Fast Market Entry Priority:
Check exemption status first
Consider Class I redesign if borderline Class II
Minimize regulatory burden for initial launch
Premium Positioning Strategy:
FDA clearance/approval adds credibility
Hospitals prefer FDA-cleared devices
Insurance reimbursement often requires FDA status
Global Market Strategy:
FDA clearance facilitates international approvals
CE marking may require FDA predicate
Consider regulatory harmonization benefits
Risk Assessment Considerations
Business Risk Tolerance:
Exempt devices have minimal regulatory protection
510(k) clearance provides competitive moat
PMA approval creates significant barriers to entry
Liability and Insurance:
Professional liability insurance rates vary by FDA status
Product liability coverage easier with FDA clearance
Clinical evidence requirements affect risk exposure
Red Flags: When You Definitely Need Professional Help
Complex Classification Scenarios
Combination Products: Drug-device, biologic-device combinations require specialized expertise
Novel Technologies: AI, nanotechnology, 3D printing often have unclear regulatory paths
Multiple Indications: Different uses may require different regulatory approaches
Borderline Cases
Class I vs. Class II: Risk-based determination can be subjective
510(k) vs. PMA: Substantial equivalence determination requires expert analysis
Exempt vs. Non-Exempt: Partial limitations and special circumstances apply
International Considerations
Global Harmonization: FDA decisions affect CE marking and other approvals
Export Requirements: Some countries require FDA clearance regardless of exemption
Manufacturing Location: Domestic vs. international manufacturing affects requirements
The Fastest Path to Market
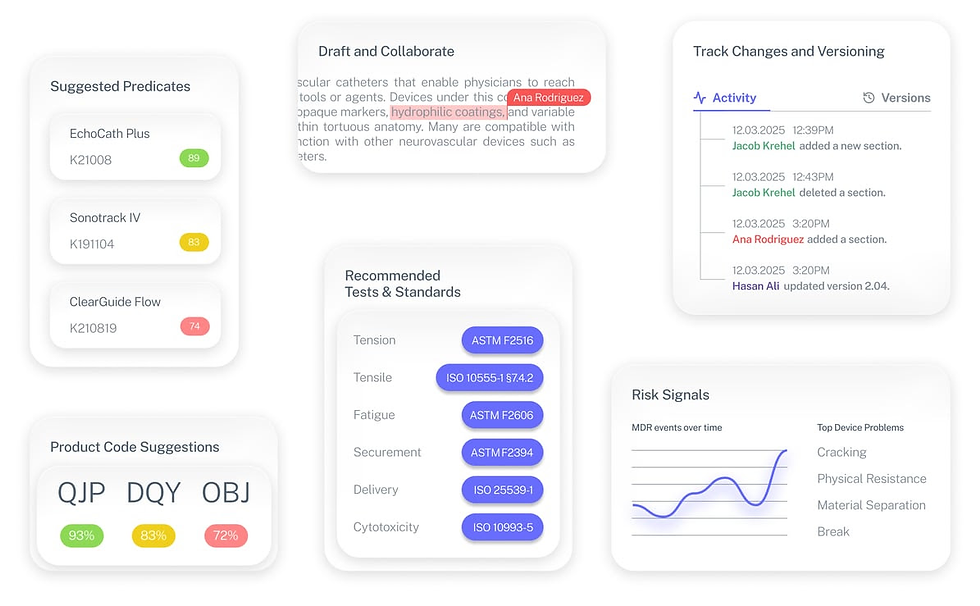
No more guesswork. Move from research to a defendable FDA strategy, faster. Backed by FDA sources. Teams report 12 hours saved weekly.
FDA Product Code Finder, find your code in minutes.
510(k) Predicate Intelligence, see likely predicates with 510(k) links.
Risk and Recalls, scan MAUDE and recall patterns.
FDA Tests and Standards, map required tests from your code.
Regulatory Strategy Workspace, pull it into a defendable plan.
👉 Start free at complizen.ai
Frequently Asked Questions
Can I sell my device while waiting for FDA clearance?
No, you cannot commercially distribute devices requiring 510(k) clearance until you receive FDA authorization. However, you can conduct clinical testing under IDE regulations.
What if I disagree with FDA's device classification?
You can request reclassification through FDA's De Novo pathway or submit a 513(g) request for classification clarification before developing your regulatory strategy.
Do exempt devices need design controls?
Most Class I devices don't require design controls per 21 CFR 820.30, but we recommend implementing them for quality assurance and international market access.
Can I change my regulatory pathway after starting?
Yes, but it often requires starting over with new documentation and may significantly delay market entry. Choose carefully from the beginning.
How often do exemption statuses change?
FDA reviews exemption lists every 5 years under the Cures Act. Monitor Federal Register notices for updates that might affect your device.


