ISO 14971:2019 Risk Management for Medical Devices: 2025 Implementation Guide
- Beng Ee Lim

- Jul 17, 2025
- 10 min read
Updated: Sep 7, 2025
ISO 14971:2019 is the international standard that defines the lifecycle risk-management process for medical devices (including SaMD): identify hazards, estimate/evaluate risk, implement/verify risk controls, and monitor production & post-production information to keep risks under control. Use ISO/TR 24971:2020 for practical methods and documentation tips; FDA aligns through ISO 13485/QMSR and recommends ISO 14971 in software submissions.
This comprehensive guide provides medical device manufacturers with practical implementation strategies, ensuring regulatory compliance while improving product safety and development efficiency.

ISO 14971:2019 vs 2007: Critical Changes You Must Know
The 2019 edition introduced fundamental changes that many manufacturers still haven't fully implemented:
Major Structural Changes
New Chapter Organization:
Grew from 9 to 10 main clauses
Enhanced clarity in risk management process steps
Improved alignment with ISO 13485 requirements
Better integration guidance for quality management systems
Benefit-Risk Analysis Introduction: The 2019 standard introduces the concept of medical benefit and requires manufacturers to perform benefit-risk analysis when risks cannot be reduced to acceptable levels through design or protective measures.
Key Definition - Medical Benefit: "Positive impact or desirable outcome of the use of a medical device on the health of an individual, or a positive impact on patient management or public health."
Enhanced Post-Market Requirements
Continuous Monitoring Obligations:
Systematic collection and analysis of post-market data
Regular review of risk management activities
Updated risk assessments based on field experience
Documentation of risk management effectiveness
Information Sources for Post-Market Surveillance:
Customer complaints and feedback
Field corrective actions and recalls
Clinical data and adverse events
Manufacturing and quality data
Regulatory reporting requirements
Risk Control Hierarchy Clarification
Updated Risk Control Measures (in priority order):
Inherent safety by design - Eliminate hazards through design
Protective measures - Reduce risks through safety systems
Information for safety - Warnings, training, and instructions
This hierarchy emphasizes that information alone cannot adequately control high-severity risks.
ISO 14971 Implementation Framework: Step-by-Step Process
ISO 14971 serves as the cornerstone of medical device safety management globally. Risk management is a regulatory requirement—without performing risk management and meeting the requirements of ISO 14971, the doors to most major medical device markets worldwide, including the US and EU, are closed.
The standard defines risk as "the combination of the probability of occurrence of harm and the severity of that harm," focusing specifically on patient safety rather than business risks. It covers all medical device types, including Software as a Medical Device (SaMD) and in vitro diagnostic (IVD) devices.
Phase 1: Risk Management Planning (Weeks 1-2)
1.1 Establish Risk Management Policy
Define organizational commitment to risk management
Assign competent personnel and resources
Establish risk acceptability criteria
Create risk management procedures
1.2 Risk Management Plan Development
Identify applicable standards and regulations
Define device intended use and reasonably foreseeable misuse
Establish risk management activities and timelines
Create risk management file structure
1.3 Risk Acceptability Criteria
Organizations must establish objective criteria for determining acceptable risk levels. The standard doesn't specify acceptable risk levels—manufacturers must define these based on:
Device classification and intended use
State-of-the-art practices for similar devices
Regulatory requirements and guidance
Clinical evidence and literature
Phase 2: Risk Analysis (Weeks 3-6)
2.1 Hazard Identification Systematic identification of potential hazards associated with the device:
Common Medical Device Hazards:
Biological hazards: Biocompatibility, infection, toxicity
Chemical hazards: Material toxicity, degradation products
Physical hazards: Mechanical failure, sharp edges, entrapment
Electrical hazards: Shock, burns, electromagnetic interference
Thermal hazards: Excessive heat, cold injury
Radiation hazards: Ionizing and non-ionizing radiation
2.2 Risk Estimation For each identified hazard, estimate:
Probability of occurrence: How likely is the hazardous situation?
Severity of harm: What are the potential consequences?
Risk level: Combination of probability and severity
Risk Estimation Methods:
Qualitative assessment (Low, Medium, High)
Semi-quantitative scoring (1-5 scales)
Quantitative analysis (when data available)
Fault tree analysis for complex systems
Failure mode and effects analysis (FMEA)
Phase 3: Risk Evaluation (Weeks 7-8)
3.1 Risk Acceptability Assessment
Compare estimated risks against predetermined acceptability criteria:
Broadly acceptable: Risks requiring no further action
Tolerable: Risks requiring risk control measures
Unacceptable: Risks requiring immediate action before use
3.2 Risk Control Decision Making
For risks that aren't broadly acceptable:
Apply risk control measures according to hierarchy
Perform benefit-risk analysis if risks remain high
Document rationale for risk acceptability decisions
Phase 4: Risk Control (Weeks 9-12)
4.1 Risk Control Measure Implementation
Apply control measures following the established hierarchy:
Inherent Safety by Design Examples:
Use biocompatible materials
Implement fail-safe mechanisms
Design connectors that prevent misconnection
Eliminate sharp edges and pinch points
Protective Measures Examples:
Install safety interlocks and alarms
Implement software safety features
Add protective barriers or guards
Include automatic shut-off mechanisms
Information for Safety Examples:
Comprehensive instructions for use
Training requirements for users
Warning labels and symbols
Contraindications and precautions
4.2 Risk Control Effectiveness Verification
Verify that control measures reduce risk as intended
Ensure control measures don't introduce new hazards
Document verification methods and results
Update risk analysis based on control measure effectiveness
Phase 5: Residual Risk Evaluation (Weeks 13-14)
5.1 Residual Risk Assessment
After implementing control measures, re-evaluate remaining risks:
Calculate residual risk levels
Compare against acceptability criteria
Perform benefit-risk analysis if needed
Document residual risk acceptability rationale
5.2 Benefit-Risk Analysis
When residual risks aren't acceptable, perform benefit-risk analysis:
Identify and quantify medical benefits
Compare benefits against residual risks
Determine if benefits outweigh risks
Document analysis methodology and conclusions
Phase 6: Risk Management Report (Week 15)
6.1 Risk Management Report Contents
Summary of risk management activities
Conclusion that residual risks are acceptable
Benefit-risk analysis results (if applicable)
Overall risk management effectiveness assessment
6.2 Risk Management Review
Independent review of risk management activities
Verification of risk management plan compliance
Assessment of risk management file completeness
Approval for product release
Integration with Quality Management Systems
ISO 14971 is designed to integrate seamlessly with ISO 13485 quality management systems:
Design and Development Integration
ISO 13485 Section 7.3.3 Requirements:
Risk management outputs must be design and development inputs, ensuring:
Risks are considered from initial design phases
Risk control measures influence design decisions
Risk management activities are documented in design files
Risk analysis updates trigger design change controls
Design Controls and Risk Management Alignment:
Design inputs: Include risk management requirements
Design outputs: Incorporate risk control measures
Design verification: Verify risk control effectiveness
Design validation: Confirm overall risk acceptability
Design changes: Trigger risk management updates
Production and Post-Production Integration
Manufacturing Risk Management:
Production process risk analysis
Supplier risk assessment and control
Non-conforming product risk evaluation
Corrective and preventive action (CAPA) integration
Post-Market Surveillance Integration:
Complaint handling and risk assessment
Field corrective actions and risk updates
Vigilance reporting and risk communication
Management review of risk management effectiveness
Post-Market Surveillance Requirements
The 2019 edition significantly enhanced post-market surveillance obligations:
Continuous Monitoring System
Required Data Collection:
Customer complaints and user feedback
Field corrective actions and recalls
Clinical performance data
Manufacturing and quality issues
Regulatory actions and communications
Data Analysis Requirements:
Trend analysis of post-market information
Pattern recognition for emerging risks
Risk-benefit evaluation updates
Effectiveness assessment of risk controls
Risk Management Updates
Triggers for Risk Management Review:
New hazard identification
Changes in risk occurrence rates
Severity assessment modifications
Risk control measure effectiveness issues
Update Process:
Re-evaluate risk analysis based on new data
Update risk control measures if needed
Revise benefit-risk analysis if applicable
Document changes in risk management file
Common Implementation Mistakes and How to Avoid Them
Mistake 1: Late Risk Management Implementation
Problem: Conducting risk management activities late in design process
Solution: Integrate risk management from initial design phases
Best Practice: Include risk management in design planning and all design reviews
Mistake 2: Inadequate Hazard Identification
Problem: Missing hazards due to limited analysis scope
Solution: Use systematic hazard identification methods
Best Practice: Involve multidisciplinary teams including clinicians, engineers, and regulatory experts
Mistake 3: Poor Risk Acceptability Criteria
Problem: Vague or inconsistent risk acceptability criteria
Solution: Establish clear, objective criteria based on device type and intended use
Best Practice: Benchmark against similar devices and regulatory expectations
Mistake 4: Insufficient Post-Market Activities
Problem: Treating risk management as one-time design activity
Solution: Implement continuous post-market surveillance system
Best Practice: Establish systematic data collection and analysis processes
Mistake 5: Inadequate Documentation
Problem: Incomplete or poorly organized risk management files
Solution: Maintain comprehensive, traceable documentation
Best Practice: Use standardized templates and document management systems

Risk Management Tools and Techniques
Hazard Identification Methods
Preliminary Hazard Analysis (PHA):
Early-stage hazard identification
High-level risk screening
Suitable for concept and design phases
Failure Mode and Effects Analysis (FMEA):
Systematic analysis of failure modes
Quantitative risk assessment capability
Excellent for design and process analysis
Fault Tree Analysis (FTA):
Top-down approach to hazard analysis
Useful for complex systems
Identifies combinations of failures
Hazard and Operability Study (HAZOP):
Systematic examination of process deviations
Effective for manufacturing process analysis
Identifies operational hazards
Risk Assessment Tools
Risk Matrices:
Simple probability vs. severity assessment
Visual risk level communication
Suitable for qualitative analysis
Monte Carlo Simulation:
Quantitative risk assessment
Handles uncertainty and variability
Useful for complex risk scenarios
Bow-Tie Analysis:
Combines fault tree and event tree analysis
Shows risk control measure effectiveness
Excellent for communication and training
Software as Medical Device (SaMD) Considerations
ISO 14971:2019 specifically addresses SaMD applications:
SaMD Risk Management Approach
Software-Specific Hazards:
Algorithm errors and computational failures
Data integrity and security issues
User interface and usability problems
Integration and interoperability risks
SaMD Risk Control Measures:
Software verification and validation
Cybersecurity and data protection
User training and competency requirements
Software maintenance and updates
Post-Market Surveillance for SaMD:
Software performance monitoring
User feedback and error reporting
Cybersecurity incident tracking
Algorithm performance validation
Integration with IEC 62304
Software Lifecycle Process Integration:
Risk management inputs to software planning
Hazard analysis during software design
Risk control through software architecture
Post-market surveillance of software performance
Global Regulatory Considerations
FDA Requirements
FDA Recognition of ISO 14971:
FDA-Specific Considerations:
Emphasis on clinical risk-benefit analysis
Post-market surveillance reporting requirements
Integration with FDA's MAUDE database
Alignment with FDA guidance documents
EU MDR/IVDR Requirements
Harmonized Standard Status:
EN ISO 14971:2019+A11:2021 is harmonized with MDR/IVDR
Annex ZA demonstrates MDR compliance
Annex ZB demonstrates IVDR compliance
Presumption of conformity with General Safety and Performance Requirements
EU-Specific Requirements:
Clinical evaluation and risk management integration
Post-market clinical follow-up obligations
Vigilance reporting and risk communication
Notified body assessment of risk management
Other Global Markets
Health Canada:
ISO 14971 required for medical device licenses
Integration with Quality System Certification
Post-market surveillance reporting
TGA (Australia):
Risk management requirements for TGA registration
Alignment with Australian regulatory framework
Post-market monitoring obligations
Advanced Risk Management Strategies
Digital Health and AI/ML Devices
Unique Risk Considerations:
Algorithm bias and fairness
Data privacy and security
Continuous learning system risks
Human-AI interaction challenges
Risk Control Approaches:
Algorithm validation and testing
Data governance and quality assurance
User interface design and training
Continuous monitoring and updates
Combination Products
Multi-Disciplinary Risk Management:
Drug-device interaction risks
Integrated manufacturing controls
Combined clinical risk assessment
Coordinated post-market surveillance
Cybersecurity Risk Management
Cybersecurity Risk Integration:
Threat modeling and vulnerability assessment
Security controls and monitoring
Incident response and recovery
Supply chain security management
Risk Management File Documentation
Required Documentation Components
Risk Management Plan:
Risk management policy and procedures
Risk acceptability criteria
Risk management activities and timelines
Competent personnel assignments
Risk Analysis Documentation:
Hazard identification records
Risk estimation methodologies
Risk evaluation results
Risk control measure specifications
Risk Control Verification:
Control measure effectiveness verification
Residual risk assessment results
Benefit-risk analysis (if applicable)
Risk management report
Post-Market Surveillance Records:
Post-market data collection procedures
Risk management review results
Risk management updates and changes
Effectiveness monitoring data
Documentation Best Practices
Traceability Requirements:
Link risks to specific device components
Trace control measures to risk analysis
Connect post-market data to risk updates
Maintain version control and change history
Review and Approval Process:
Independent review of risk management activities
Competent personnel approval requirements
Management review integration
Audit trail maintenance
Measuring Risk Management Effectiveness
Performance Indicators
Leading Indicators:
Hazard identification completeness
Risk assessment accuracy
Control measure implementation timeliness
Training effectiveness metrics
Lagging Indicators:
Post-market incident rates
Field corrective action frequency
Customer satisfaction scores
Regulatory inspection findings
Continuous Improvement
Risk Management System Review:
Annual risk management effectiveness assessment
Benchmarking against industry performance
Process improvement identification
Technology and method updates
Organizational Learning:
Cross-product risk management lessons
Industry best practice adoption
Regulatory expectation updates
Competency development programs
Strategic Implementation Recommendations
Organizational Readiness
Resource Requirements:
Dedicated risk management personnel
Cross-functional team involvement
Training and competency development
Technology and tool investments
Cultural Transformation:
Risk-aware decision making
Proactive hazard identification
Continuous improvement mindset
Regulatory compliance commitment
Phased Implementation Approach
Phase 1: Foundation Building (Months 1-3)
Establish risk management policy and procedures
Train personnel on ISO 14971 requirements
Set up risk management file structure
Begin pilot product risk analysis
Phase 2: System Implementation (Months 4-9)
Complete risk analysis for all products
Implement risk control measures
Establish post-market surveillance system
Conduct risk management reviews
Phase 3: Optimization and Maturity (Months 10-12)
Refine risk management processes
Implement advanced risk assessment tools
Establish continuous improvement programs
Achieve full regulatory compliance
Strategic Takeaways
ISO 14971:2019 represents a fundamental shift toward integrated, lifecycle-based risk management:
Start early - Risk management must begin in design planning phases
Think systematically - Use structured methods for hazard identification and risk assessment
Focus on post-market - Establish robust surveillance systems for continuous risk monitoring
Integrate deeply - Embed risk management throughout quality management systems
Document thoroughly - Maintain comprehensive, traceable risk management files
Improve continuously - Use post-market data to enhance risk management effectiveness
Effective risk management is not just about regulatory compliance—it's about building safer, more effective medical devices that improve patient outcomes while protecting organizations from regulatory and commercial risks.
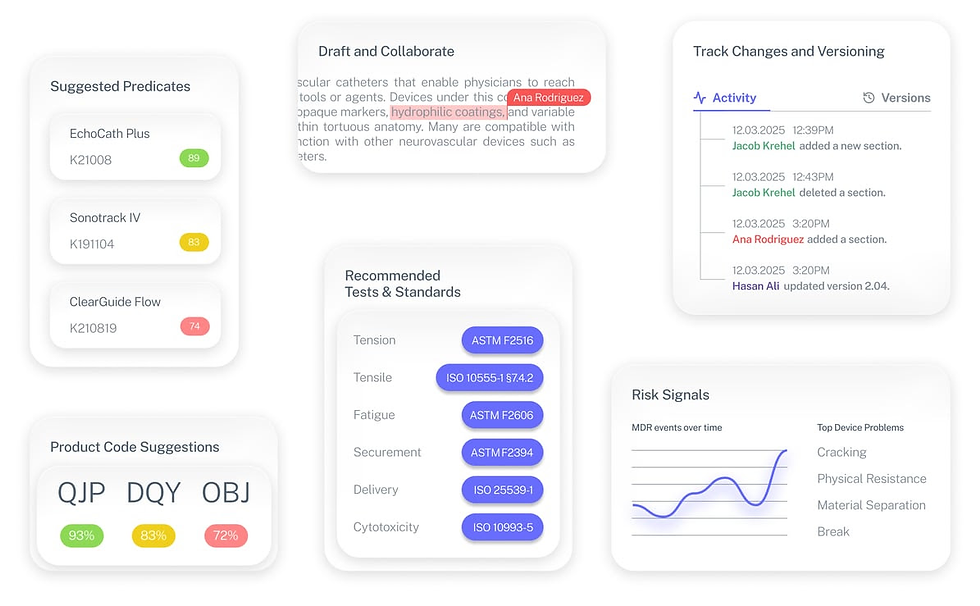
The Fastest Path to Market
No more guesswork. Move from research to a defendable FDA strategy, faster. Backed by FDA sources. Teams report 12 hours saved weekly.
FDA Product Code Finder, find your code in minutes.
510(k) Predicate Intelligence, see likely predicates with 510(k) links.
Risk and Recalls, scan MAUDE and recall patterns.
FDA Tests and Standards, map required tests from your code.
Regulatory Strategy Workspace, pull it into a defendable plan.
👉 Start free at complizen.ai
Frequently Asked Questions
Is ISO 14971 mandatory for medical devices?
While not legally required, ISO 14971 is effectively mandatory as major regulators worldwide recognize it as the standard for medical device risk management. Non-compliance significantly limits market access.
How does ISO 14971:2019 differ from the 2007 version?
Key differences include enhanced post-market surveillance requirements, benefit-risk analysis introduction, streamlined structure, and stronger integration with quality management systems.
What's the relationship between ISO 14971 and ISO 13485?
ISO 13485 requires risk management integration throughout the quality management system. ISO 14971 provides the specific methodology for medical device risk management.
How often should risk management activities be updated?
Risk management should be updated whenever new hazards are identified, risk control effectiveness changes, or significant post-market data becomes available. Regular reviews are recommended annually at minimum.
Can ISO 14971 be applied to software medical devices?
Yes, ISO 14971:2019 specifically addresses Software as Medical Device (SaMD) applications and should be integrated with IEC 62304 software lifecycle processes.


