Top Reasons SaMD 510(k)s Get AI Letters (and How to Fix Them)
- Beng Ee Lim

- Jun 24, 2025
- 7 min read
Updated: Sep 7, 2025
Most SaMD 510(k)s hit a first-cycle Additional Information (AI) letter, not a final rejection. The recurring issues: missing cybersecurity materials (for §524B cyber devices), thin AI/ML evidence (data lineage, generalizability, validation), and weak predicate comparisons. Fix them by aligning to FDA’s DSF software guidance, 2025 AI draft, and 2025 cyber final—organized in eSTAR.
In this article we'll break down FDA requirements and the complex nature of software validation, and the best practices to ensure 510(K) success for SaMD.

At a Glance: SaMD 510(k) Rejection Landscape
Top Rejection Category | Impact Level | 2025 Enforcement |
Cybersecurity Gaps | Critical | Mandatory since Oct 2023 |
AI/ML Validation Issues | High | Enhanced scrutiny |
Predicate Equivalence Problems | Critical | Ongoing challenge |
Documentation Inconsistencies | Medium | Standard enforcement |
Clinical Validation Gaps | Medium | Increasing focus |

The Current SaMD Rejection Reality
The FDA cleared 691 AI/ML-enabled medical devices as of October 2023, with the majority going through the 510(k) pathway. However, rejection rates remain concerningly high due to the unique challenges software presents compared to traditional hardware devices.
Key Industry Context:
Over 37% of cleared AI/ML devices originated from non-AI/ML predicates, creating substantial equivalence challenges
Early FDA summaries called out “AI” in only 45 % of approvals, fueling classification confusion.
Nearly half of FDA-approved AI devices lack robust clinical validation data
1. Cybersecurity and SBOM Compliance Failures
The New Reality
FDA began refusing to accept any cyber-device submission that lacks a full SBOM, threat model or patch plan on 1 Oct 2023. As a result, cyber gaps are now the most common automatic RTA trigger for connected SaMD files.
Most Common Cybersecurity Rejection Reasons:
Missing Software Bill of Materials (SBOM)
Incomplete inventory of software components
Failure to identify third-party and open-source components
Missing version numbers and vulnerability assessments
Inadequate Cybersecurity Risk Assessment
Submission of plans outlining how the company will track and address cybersecurity issues that occur after the device is on the market not provided
Insufficient threat modeling for "cyber devices"
Missing penetration testing results
Post-Market Monitoring Plans
No defined process for vulnerability tracking
Unclear incident response procedures
Missing update and patch deployment strategies
2. AI/ML Validation and Predicate Equivalence Issues
The Predicate Problem
More than a third of cleared AI/ML-based medical devices originated from non-AI/ML-based medical devices in the first generation, creating substantial equivalence challenges that frequently lead to rejections.
Common AI/ML Rejection Patterns:
Inappropriate Predicate Selection
Claiming equivalence to non-AI devices for AI-enabled functions
Devices with the longest time since the last predicate device with an AI/ML component were haematology (2001), radiology (2001), and cardiovascular devices (2008).
Mismatched intended use statements between AI and non-AI predicates.
Insufficient Algorithm Validation
Missing training data demographics and bias assessment
Inadequate performance testing across diverse populations
Clinical Study Participants and Data Sets Are Representative of the Intended Patient Population not demonstrated
Algorithm Change Control Issues
No predetermined change control plan (PCCP) for continuous learning algorithms
Unclear retraining triggers and validation processes
Missing performance monitoring metrics
3. Documentation Level Misalignment
The Two-Tier Challenge
The FDA uses a risk-based approach to determine the level of detail required in a software medical device's documentation. This approach ensures that devices with higher risks (Enhanced) undergo more scrutiny, while low-risk (Basic) devices can provide less documentation.
Common Documentation Failures:
Wrong Documentation Level Selection
Choosing Basic when Enhanced is required
Insufficient risk assessment to justify documentation level
Missing Software Design Specification (SDS) for Enhanced submissions
Architecture and Design Gaps
Enhanced: Provide layered diagrams with details on: Interfaces and interdependencies between software modules. Data inputs, outputs, and flow paths. Cybersecurity architecture and measures to mitigate risks not provided
Inadequate software architecture documentation
Missing data flow and security diagrams
Traceability Issues
Poor linkage between requirements, design, and testing
Missing risk-to-control traceability
Inadequate change management documentation
Pro tip: If your SaMD touches patients directly, uses AI/ML, connects to the cloud, or forms part of a combination product, assume Enhanced is mandatory—and build the SDS, architecture, and traceability matrix before you draft the 510(k).
4. Clinical Validation and Real-World Evidence Gaps
The Clinical Data Challenge
Almost half of FDA-approved medical AI devices lack clinical validation data, yet the FDA is increasingly demanding robust clinical evidence for SaMD submissions.
Clinical Validation Rejection Reasons:
Insufficient Clinical Evidence
Missing prospective clinical studies
Retrospective data without appropriate controls
Performance metrics not clinically meaningful
Population Representation Issues
Only 14.5% of devices provided race or ethnicity data
Inadequate demographic diversity in training/testing datasets
Missing pediatric considerations where applicable
Performance Metric Problems
Using technical metrics instead of clinical outcomes
Missing sensitivity/specificity in real-world conditions
Inadequate comparison to clinical standard of care
Bottom line: pair solid demographics with prospective, clinically relevant studies—and lock them to a robust PCCP—if you want your AI 510(k) to survive first review.
5. Indication for Use and Labeling Inconsistencies
The Consistency Problem
This is one of the biggest reasons FDA rejects 510(k) submissions - inconsistent Indication for Use (IFU) statements appearing throughout the submission.
Common IFU-Related Rejections:
Software-Specific Labeling Issues
Unclear software function descriptions
Missing AI/ML algorithm limitations
Inadequate user interface specifications
Clinical Decision Support vs. Diagnostic Claims
Confusion between CDS and CADx (Computer-Aided Diagnosis) devices
Inappropriate diagnostic claims for decision support tools
Missing physician oversight requirements
Performance Claims Misalignment
Laboratory performance vs. clinical performance confusion
Overstated algorithm capabilities
Missing performance limitations and warnings
Fix it: copy-paste your IFU verbatim into every section, keep claims inside proven performance, and use FDA’s CDS flowchart if there’s any doubt about diagnostic language.
6. Software Lifecycle and Quality Management Deficiencies
The Process Problem
Good Software Engineering and Security Practices Are Implemented - FDA increasingly scrutinizes software development processes for SaMD submissions.
Process-Related Rejection Reasons:
IEC 62304 Compliance Gaps
Missing software lifecycle process documentation
Inadequate software safety classification
Poor change control procedures
Design Controls Deficiencies
Missing Design History File (DHF) elements
Inadequate software requirements specifications
Poor verification and validation documentation
Risk Management Issues
ISO 14971 implementation gaps
Missing software-specific hazard analysis
Inadequate risk control effectiveness verification
Pro tip: assume reviewers will ask to see your IEC 62304 mapping table, risk file, and change-control SOP—have them ready before you click “Submit.”
Emerging Rejection Trends in 2025
1. Enhanced AI/ML Scrutiny
Jan 2025 draft guidance demands a total-product-lifecycle plan, algorithm-transparency docs and a rock-solid continuous-monitoring / PCCP. Miss any one and reviewers bounce the file.
2. Interoperability and Integration Issues
With FDA exploring FHIR-based study data, SaMD files now get quizzed on FHIR mapping, EHR-integration test results and API security hardening. Treat this as the next cyber-checklist item.
3. Human Factors Engineering Gaps
Submissions lacking UI usability studies, error-mitigation analysis or workflow fit run afoul of FDA’s HF/UE guidance.
Take-away: 2025 reviewers expect SaMD 510(k)s to show airtight AI lifecycle control, speak FHIR when data cross systems, and prove a clinician can’t click the wrong button in real life. Shore up those three areas before you press “submit.”
Industry-Specific Rejection Patterns
Radiology SaMD (Highest Volume, Highest Scrutiny)
Most Common Issue: AI/ML tasks changed frequently along the device's predicate network, raising safety concerns
Key Challenge: Demonstrating equivalence when moving from image processing to AI interpretation
Frequent Rejection: Inadequate DICOM compliance and integration testing
Cardiovascular SaMD
Primary Issue: Clinical validation in diverse patient populations
Common Gap: Missing real-world performance data
Frequent Problem: Inadequate rhythm analysis validation
Digital Therapeutics
Main Challenge: Establishing appropriate predicate devices
Key Issue: Clinical efficacy demonstration
Common Failure: Missing behavioral outcome validation

Prevention Strategies: Learning from Rejections
1 — Start with a Pre-Sub
Book a Q-Submission 4-12 months before you file. Bring your predicate logic and a high-level cyber-architecture diagram so FDA can spot gaps early.
2 — Match docs to risk
Use the 2023 Software-Content guidance: Basic vs Enhanced documentation hinges on patient risk. When unsure, over-deliver—Enhanced needs an SDS, layered architecture, and full traceability.
3 — Build security in
Create the SBOM as you code, run routine pentests, and draft a post-market patch plan; §524B lets FDA refuse “cyber-devices” missing these items.
4 — Follow GMLP for AI/ML
Adopt FDA’s 10 Good-ML principles, include a Predetermined Change Control Plan, and show bias-checked, diverse training data.
5 — Prove it clinically
Design prospective, multi-site studies with meaningful endpoints and run real-world validation in the intended workflow.
Lock these five habits in, and most “automatic” RTA triggers evaporate before your SaMD dossier even hits FDA’s inbox.
Key Takeaways for SaMD Companies
The rejection landscape for SaMD 510(k)s is evolving rapidly, with cybersecurity and AI/ML validation issues dominating recent patterns. Companies that proactively address these challenges through early FDA engagement, robust technical documentation, and comprehensive validation strategies significantly improve their approval odds.
Critical Success Factors:
Cybersecurity compliance is non-negotiable - ensure SBOM and post-market plans are comprehensive
Predicate strategy requires careful consideration - non-AI predicates create substantial equivalence challenges
Clinical validation is increasingly important - retrospective data alone is often insufficient
Documentation consistency matters - automated checking can prevent common IFU errors
Early FDA engagement pays dividends - Q-Sub meetings help identify potential issues before submission
The Bottom Line: SaMD rejections are largely preventable with proper preparation, but the bar continues to rise. Companies that invest in comprehensive regulatory strategy and leverage modern compliance tools will have significant advantages in this competitive landscape.
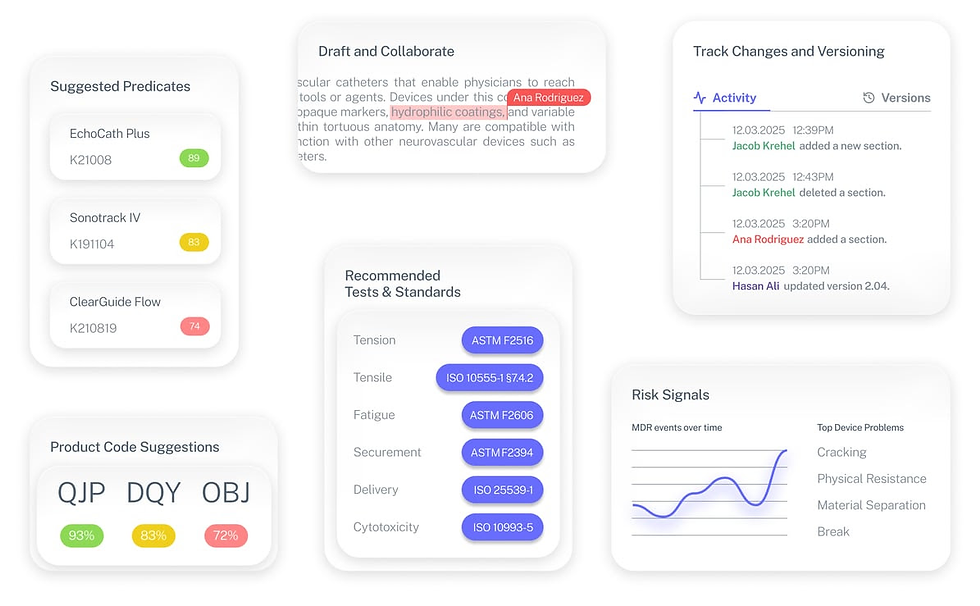
The Fastest Path to Market
No more guesswork. Move from research to a defendable FDA strategy, faster. Backed by FDA sources. Teams report 12 hours saved weekly.
FDA Product Code Finder, find your code in minutes.
510(k) Predicate Intelligence, see likely predicates with 510(k) links.
Risk and Recalls, scan MAUDE and recall patterns.
FDA Tests and Standards, map required tests from your code.
Regulatory Strategy Workspace, pull it into a defendable plan.
👉 Start free at complizen.ai
Frequently Asked Questions
Q: What's the current rejection rate for SaMD 510(k) submissions?
A: While specific SaMD rejection rates aren't publicly disclosed, industry experts estimate 60-75% of first-time SaMD submissions receive major deficiency letters or rejections, similar to overall 510(k) rates.
Q: How has cybersecurity enforcement changed rejection patterns?
A: Since October 2023, cybersecurity deficiencies have become the leading cause of immediate RTA decisions, with incomplete SBOMs and missing post-market monitoring plans being primary issues.
Q: Can AI/ML devices use non-AI predicates for 510(k) clearance?
A: Yes, but this approach is increasingly challenging. The FDA scrutinizes whether AI components represent "different technological characteristics" that could affect safety and effectiveness.
Q: What's the biggest mistake SaMD companies make in 510(k) submissions?
A: Underestimating the documentation requirements and failing to engage with FDA early in the development process. Most successful SaMD companies schedule Q-Sub meetings well before submission.
Q: How long do SaMD 510(k) reviews typically take?
A: Standard 510(k) reviews target 90 days, but SaMD submissions often require additional information requests, extending timelines to 4-8 months for complex AI/ML devices.
Stay ahead of evolving SaMD regulations with Complizen's AI-powered compliance platform. Our regulatory intelligence system helps medical device companies navigate complex requirements and avoid common submission pitfalls.


