Predetermined Change Control Plan (PCCP) for AI/ML-Enabled Devices: 2025 FDA Guide
- Beng Ee Lim

- Aug 6, 2025
- 10 min read
Updated: Sep 7, 2025
A Predetermined Change Control Plan (PCCP) is FDA documentation that lets you pre-define specific AI/ML software changes—and the methods to develop, validate, implement, and monitor them—so those updates can be made without a new marketing submission, when executed exactly as an authorized PCCP. PCCPs include three components: Description of Modifications, Modification Protocol, and Impact Assessment. Available for 510(k), De Novo, and PMA pathways for AI-enabled device software functions.
This guide covers the final December 2024 FDA guidance requirements, implementation strategies, and practical examples for successful PCCP development.

What Is a Predetermined Change Control Plan (PCCP)?
A Predetermined Change Control Plan is a regulatory framework that allows manufacturers to implement pre-approved modifications to AI-enabled medical devices without submitting supplemental marketing applications for each change. This approach addresses the iterative nature of AI/ML development while maintaining safety and effectiveness standards.
Why PCCPs Are Essential for AI Medical Devices
Traditional Change Control Limitations: Conventional medical device change control requires new submissions (Special 510(k), PMA supplement) for significant software modifications. For AI devices that continuously learn and improve, this creates regulatory bottlenecks that can delay critical updates.
PCCP Strategic Advantages:
Continuous Innovation: Implement AI improvements without regulatory delays
Cost Reduction: Eliminate expensive supplemental submission cycles
Competitive Edge: Deploy algorithmic enhancements faster than competitors
Patient Benefit: Accelerate delivery of improved diagnostic accuracy and treatment outcomes
FDA Regulatory Authority
The FDA's PCCP authority stems from the Food and Drug Omnibus Reform Act (FDORA) of 2022, which added section 515C to the Federal Food, Drug, and Cosmetic Act. This provides express statutory authority for FDA to authorize predetermined change control plans as part of initial marketing submissions.
AI-DSF Definition and Scope
Updated FDA Terminology (2025)
The final FDA guidance transitioned from "Machine Learning-Enabled Device Software Functions (ML-DSF)" to "Artificial Intelligence-Enabled Device Software Functions (AI-DSF)" to reflect broader AI application scope.
FDA AI Definition: "A machine-based system that can, for a given set of human-defined objectives, make predictions, recommendations, or decisions influencing real or virtual environments."
AI-DSF Definition: "A device software function that implements an AI model" and includes various AI techniques beyond just machine learning algorithms.
PCCP Applicability
Devices Eligible for PCCP:
AI-enabled medical devices across all risk classifications
Device-led combination products with AI-DSF components
Software as Medical Device (SaMD) with AI functionality
Traditional medical devices with embedded AI algorithms
Regulatory Pathways:
510(k) Premarket Notification: Most common pathway for AI device modifications
De Novo Classification Request: Novel AI devices establishing new device classifications
PMA Applications: High-risk AI devices requiring comprehensive safety and effectiveness data
Exclusions:
Minor software maintenance that doesn't affect safety or effectiveness (covered under Quality System Regulation)
Changes to drug or biologic components of combination products
Modifications outside the original device intended use without specific justification
Three Essential PCCP Components
Component 1: Description of Modifications
This section specifies exactly what changes will occur to the AI-DSF and their expected impact on device performance.
Required Elements:
Specific Modification Types:
Algorithm parameter adjustments and threshold modifications
Training data updates and model retraining procedures
Performance metric improvements (sensitivity, specificity, accuracy)
User interface enhancements that affect AI functionality
Integration updates for interoperable system compatibility
Device Characteristic Changes:
Quantified performance improvements with statistical bounds
Changes to device outputs, alerts, or recommendations
Modifications to data input requirements or processing methods
Updates to risk mitigation measures or safety controls
Implementation Approach:
Automatic updates through software deployment systems
Manual updates requiring healthcare provider intervention
Hybrid approaches with user confirmation requirements
Rollback procedures for unsuccessful modifications
Example Description: "The AI-DSF will implement algorithm parameter adjustments to improve diagnostic accuracy for detecting diabetic retinopathy in retinal images. Modifications include sensitivity threshold adjustments (±5%), specificity optimization (target >95%), and integration of additional training data representing diverse patient populations. Updates will be deployed automatically with healthcare provider notification and 30-day performance monitoring period."
Component 2: Modification Protocol
This section details the systematic approach for developing, validating, and implementing the planned modifications.
Development Methodology:
Data Management Procedures:
Training data collection and validation protocols
Data quality assessment and bias evaluation methods
Dataset versioning and change documentation procedures
Performance monitoring data collection and analysis plans
Validation and Testing Requirements:
Pre-deployment testing protocols with acceptance criteria
Clinical validation methods for performance verification
Real-world performance monitoring and assessment procedures
Failure detection and response mechanisms
Implementation Controls:
Change authorization and approval workflows
Deployment scheduling and rollout procedures
User notification and training requirements
Documentation and audit trail maintenance
Quality Assurance Integration:
Integration with existing Quality Management System (QMS)
Design control procedures for modification management
Risk management updates and assessment protocols
Corrective and Preventive Action (CAPA) procedures for modification failures
Example Protocol: "Algorithm modifications will be validated using a holdout test dataset of 10,000 retinal images with confirmed diagnoses. Performance criteria require sensitivity ≥90% and specificity ≥95% with 95% confidence intervals. Successful validation triggers automated deployment with real-time performance monitoring for 30 days. Any performance degradation >5% triggers automatic rollback to previous algorithm version."
Component 3: Impact Assessment
This section evaluates the potential effects of planned modifications on device safety, effectiveness, and benefit-risk profile.
Safety Impact Analysis:
Patient Safety Considerations:
Potential for false positive/negative results and clinical consequences
Changes to diagnostic accuracy and treatment decision impact
Risk mitigation measures for modification failures
User training requirements for modified device functionality
Clinical Effectiveness Assessment:
Expected improvements to patient outcomes and diagnostic accuracy
Quantified performance metrics with statistical confidence intervals
Clinical workflow integration and healthcare provider impact
Long-term monitoring and assessment procedures
Risk-Benefit Analysis:
Detailed risk assessment using ISO 14971 methodology
Benefit quantification with clinical outcome improvements
Risk mitigation strategies and control measures
Post-market surveillance and monitoring plans
Stakeholder Impact:
Healthcare provider training and workflow modification requirements
Patient communication about device updates and performance changes
Integration impact on healthcare IT systems and interoperability
Regulatory reporting and notification procedures
Example Assessment: "Algorithm improvements are expected to reduce false negative rates by 15%, potentially preventing 150 missed diagnoses per 10,000 screenings. Clinical benefits include earlier diabetic retinopathy detection and treatment initiation. Risks include temporary performance variation during algorithm transition, mitigated by 30-day parallel monitoring and immediate rollback capability. Healthcare providers will receive automated performance reports and modification notifications."
PCCP Development Strategy
Pre-Development Planning
Device Classification Analysis: Determine appropriate regulatory pathway based on device risk classification and AI-DSF complexity. Higher-risk devices require more comprehensive PCCP documentation and validation protocols.
Intended Use Boundary Definition: Clearly establish the scope of modifications that remain within original device intended use. Any changes that might affect indications for use require careful justification and additional regulatory consideration.
Stakeholder Engagement:
FDA Pre-Submission Meetings: Discuss PCCP strategy and obtain agency feedback
Clinical Partners: Validate modification protocols with end-users
IT Integration Teams: Ensure compatibility with healthcare system requirements
Technical Implementation
AI Model Architecture Considerations:
Modular design enabling component-level modifications
Version control systems for algorithm and training data management
Performance monitoring integration and automated testing capabilities
Rollback mechanisms for unsuccessful modifications
Data Infrastructure Requirements:
Secure data collection and storage systems for ongoing training
Performance monitoring and analytics platforms
Real-world evidence collection and analysis capabilities
Integration with existing healthcare IT systems
Quality System Integration:
Design control procedures for PCCP-covered modifications
Risk management file updates and maintenance procedures
Document control and change management protocols
Training and competency management for development teams
Regulatory Submission Preparation
Documentation Organization: Structure PCCP documentation as standalone section within marketing submission, clearly cross-referenced with device description, risk analysis, and clinical evaluation sections.
Evidence Package Development:
Historical performance data demonstrating algorithm reliability
Validation study results supporting modification protocols
Risk analysis documentation with mitigation strategies
Clinical evidence supporting expected performance improvements
FDA Interaction Strategy:
Schedule Q-Submission meetings to validate PCCP approach
Prepare responses to anticipated FDA questions about modification scope
Develop communication plan for post-market performance reporting
Establish ongoing dialogue channels for PCCP implementation updates
Common PCCP Mistakes and How to Avoid Them
Scope and Boundary Errors
Mistake: Overly broad modification descriptions that exceed intended use boundaries
Impact: FDA rejection or requests for additional clinical data
Solution: Clearly define specific, bounded modifications with quantified performance parameters
Mistake: Insufficient justification for modifications that approach indications for use changes
Impact: Regulatory delays and additional submission requirements
Solution: Provide comprehensive rationale with clinical evidence supporting safety within current intended use
Technical Implementation Failures
Mistake: Inadequate validation protocols that don't demonstrate modification effectiveness
Impact: FDA questions about modification safety and effectiveness assurance
Solution: Develop rigorous testing protocols with statistical validation and acceptance criteria
Mistake: Missing rollback procedures for unsuccessful modifications
Impact: Patient safety concerns and regulatory compliance issues
Solution: Implement automated rollback systems with performance monitoring triggers
Documentation and Process Errors
Mistake: Inconsistency between PCCP components and other submission sections
Impact: FDA confusion and additional information requests
Solution: Ensure alignment between PCCP, device description, risk analysis, and clinical evaluation
Mistake: Insufficient integration with Quality Management System procedures
Impact: Post-market compliance challenges and audit findings
Solution: Integrate PCCP procedures with existing QMS design controls and change management
Strategic Implementation by Regulatory Pathway
510(k) Submission Strategy
Substantial Equivalence Considerations:
Demonstrate that PCCP modifications maintain substantial equivalence to predicate device
Reference predicate device performance characteristics in modification boundaries
Address any performance improvements that might affect equivalence determination
Predicate Device Analysis:
Identify predicate devices with similar AI functionality and modification approaches
Compare PCCP scope with predicate device capabilities and performance
Document how modifications maintain or improve upon predicate device performance
Documentation Focus:
Emphasize modification protocol validation and testing procedures
Demonstrate robust performance monitoring and quality controls
Reference FDA consensus standards for AI device development where applicable
De Novo Request Integration
Special Controls Development:
Incorporate PCCP requirements into proposed special controls framework
Demonstrate how modification protocols support novel device classification
Establish precedent for future 510(k) submissions referencing PCCP approach
Risk-Benefit Framework:
Comprehensive risk analysis addressing novel AI device functionality
Benefit quantification with clinical evidence supporting PCCP approach
Post-market study commitments for long-term modification effectiveness assessment
Innovation Pathway Benefits:
Position PCCP as enabling technology for continuous AI device improvement
Demonstrate regulatory pathway efficiency for AI device modifications
Establish framework for similar devices in device classification
PMA Application Enhancement
Clinical Evidence Integration:
Incorporate PCCP validation data into comprehensive clinical evaluation
Design clinical studies to support modification protocol validation
Include post-market study protocols for ongoing PCCP effectiveness assessment
Manufacturing and Quality:
Demonstrate PCCP integration with manufacturing quality systems
Address scale-up considerations for modification deployment procedures
Include post-market surveillance protocols specific to PCCP modifications
Post-Market Commitments:
Establish ongoing performance monitoring and reporting requirements
Commit to regular PCCP effectiveness assessment and FDA communication
Include modification failure analysis and corrective action protocols
Post-Market Implementation
Performance Monitoring Requirements
Real-World Evidence Collection:
Continuous performance monitoring with statistical process control
Real-world effectiveness assessment compared to pre-market validation
Adverse event monitoring specific to AI-DSF modifications
User feedback collection and analysis procedures
Reporting and Communication:
Regular performance reports to FDA with modification effectiveness data
Healthcare provider communication about device updates and performance changes
Patient notification procedures for significant modification deployments
Integration with existing medical device reporting (MDR) requirements
Quality System Maintenance
Ongoing PCCP Compliance:
Regular assessment of modification protocol effectiveness
Update procedures for PCCP scope or methodology changes
Integration with corrective and preventive action (CAPA) procedures
Training and competency maintenance for PCCP implementation teams
Change Control Integration:
Coordination between PCCP modifications and traditional change control
Assessment of modifications that might exceed PCCP scope
Documentation and approval procedures for PCCP boundary modifications
Risk management file updates for implemented modifications
Continuous Improvement
PCCP Evolution:
Assessment of modification protocol effectiveness and optimization opportunities
Integration of lessons learned from modification deployments
Expansion of PCCP scope based on real-world experience and regulatory feedback
Coordination with FDA on PCCP updates and improvements
Industry Best Practices:
Participation in industry working groups on AI device modification protocols
Sharing of lessons learned and best practices with regulatory community
Contribution to standards development for AI device lifecycle management
Collaboration on real-world evidence collection and analysis methods
International Considerations
Global Regulatory Alignment
International Harmonization: FDA collaborates with Health Canada and UK MHRA on PCCP guiding principles, promoting international alignment for AI device modification management.
EU AI Act Compliance: Consider European AI Act requirements for high-risk AI systems, including conformity assessment procedures and post-market monitoring obligations.
ISO Standards Integration:
ISO/IEC 23053: Framework for AI risk management
ISO/IEC 23894: AI risk management for AI systems
IEC 62304: Medical device software lifecycle processes with AI considerations
Multi-Market Strategy
Coordinated Submission Planning:
Develop PCCPs that address multiple regulatory jurisdiction requirements
Plan modification protocols that support global device deployment
Coordinate with international regulatory bodies on PCCP acceptance and implementation
Regional Adaptation:
Modify PCCP components to address specific regional regulatory requirements
Include local clinical evidence and validation data where required
Address cultural and healthcare system differences in modification deployment
Future Trends and Considerations
Regulatory Evolution
Expanded PCCP Scope: FDA considering expansion of PCCP framework beyond AI devices to other software-intensive medical devices requiring frequent updates.
Enhanced Automation: Development of automated PCCP assessment and approval procedures using regulatory science and AI tools for submission review.
Real-World Evidence Integration: Increased emphasis on real-world evidence collection and analysis to support PCCP modification effectiveness and safety assessment.
Technology Integration
Advanced AI Techniques:
Federated learning implementations with distributed model training
Continuous learning systems with automated performance optimization
Explainable AI requirements for modification transparency and validation
Interoperability Standards:
FHIR integration for AI device data exchange and modification coordination
HL7 standards for AI device modification notification and reporting
Cloud-based modification deployment and management systems
Implementation Checklist
Pre-Submission Phase
Strategic Planning:
Assess device eligibility for PCCP framework
Define modification scope and boundaries within intended use
Identify regulatory pathway and submission strategy
Schedule FDA pre-submission meeting to discuss PCCP approach
Technical Preparation:
Design AI architecture to support planned modifications
Develop validation protocols with statistical acceptance criteria
Implement performance monitoring and rollback systems
Integrate PCCP procedures with quality management system
PCCP Development
Documentation Preparation:
Complete Description of Modifications with quantified parameters
Develop comprehensive Modification Protocol with validation procedures
Conduct thorough Impact Assessment with risk-benefit analysis
Ensure consistency across all PCCP components and submission sections
Validation and Testing:
Execute modification protocol validation studies
Demonstrate rollback and failure response procedures
Validate performance monitoring and assessment systems
Complete integration testing with existing device functionality
Post-Submission Management
FDA Interaction:
Respond to FDA questions with supporting evidence and clarification
Provide additional validation data if requested
Coordinate with FDA on modification implementation timeline
Establish ongoing communication procedures for post-market updates
Implementation Readiness:
Train implementation teams on PCCP procedures and requirements
Establish performance monitoring and reporting systems
Develop user communication and training materials
Prepare for initial modification deployment and assessment
Ready to Navigate PCCP Implementation Successfully?
Predetermined Change Control Plans represent a paradigm shift in AI medical device regulation, enabling continuous innovation while maintaining safety and effectiveness standards. Companies that master PCCP implementation will gain significant competitive advantages through faster deployment of AI improvements and reduced regulatory burden.
Smart AI medical device companies partner with regulatory experts who understand both the technical requirements and strategic opportunities of PCCP implementation.
The Fastest Path to Market
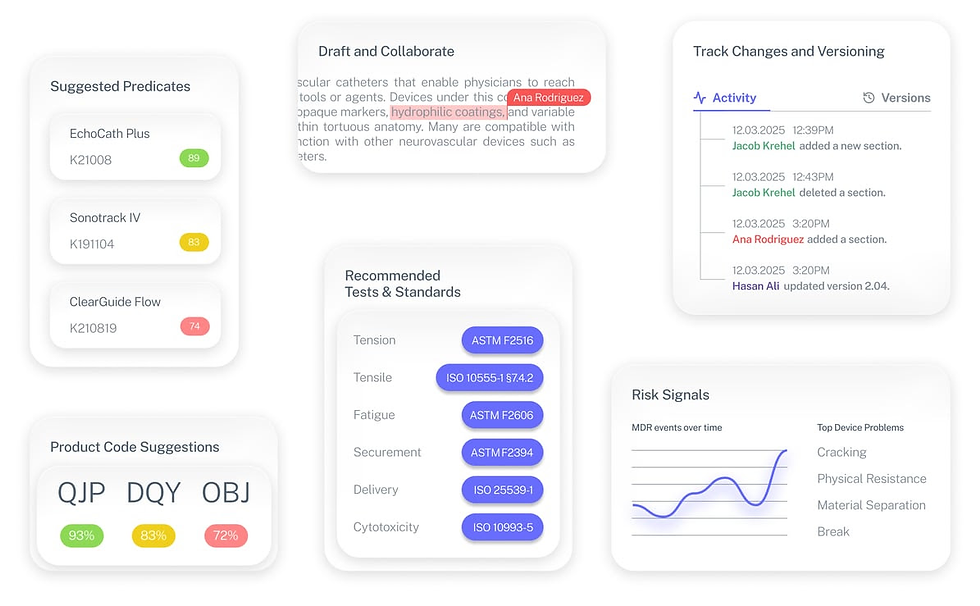
No more guesswork. Move from research to a defendable FDA strategy, faster. Backed by FDA sources. Teams report 12 hours saved weekly.
FDA Product Code Finder, find your code in minutes.
510(k) Predicate Intelligence, see likely predicates with 510(k) links.
Risk and Recalls, scan MAUDE and recall patterns.
FDA Tests and Standards, map required tests from your code.
Regulatory Strategy Workspace, pull it into a defendable plan.
👉 Start free at complizen.ai
Frequently Asked Questions
What types of AI device modifications require a PCCP versus traditional change control?
PCCP is appropriate for planned, iterative AI improvements within intended use boundaries. Traditional change control applies to unplanned changes, hardware modifications, or changes affecting device indications for use.
How does FDA review PCCP submissions differently from standard device submissions?
FDA evaluates PCCPs as part of the initial marketing submission, focusing on modification protocols, validation procedures, and impact assessments rather than reviewing each individual change.
Can we modify our PCCP after FDA approval of our initial submission?
PCCP modifications typically require supplemental submissions unless the changes are minor and within the original PCCP scope. Major PCCP changes may require new marketing submissions.
How do we handle modifications that exceed our approved PCCP scope?
Modifications outside PCCP boundaries require traditional change control procedures, potentially including Special 510(k), De Novo supplement, or PMA supplement submissions.
What happens if our PCCP modifications don't perform as expected?
PCCPs must include rollback procedures and failure response protocols. Performance monitoring requirements help identify issues early, and corrective actions should be documented and reported to FDA.


